-
结直肠癌是世界范围内常见的消化道恶性肿瘤,其发病率位于男性肿瘤的第三位,女性肿瘤的第二位。近年来随着诊治技术迅速发展,其5年生存率已经得到了很大提高[1-2]。但由于肿瘤的复发及化疗等原因,其临床疗效尚不能令人满意。因此,临床上仍然迫切需要寻求临床和生物标记物来提高结直肠癌病人的诊治效果。预后营养指数(prognostic nutritional index,PNI)是使用血清白蛋白和淋巴细胞的绝对值计算而来,最初用于评价外科病人的营养状态。近年来有研究表明PNI与肿瘤的发生发展有着密切的关系[3-4]。体质量指数(body mass index,BMI)是评价肥胖的可靠指标。最近国外有研究[5]表明BMI与食管癌的预后有关。然而目前国内外尚无研究使用PNI和BMI建立联合预测模型来评估结直肠癌病人术后预后。因此,该研究探讨PNI和BMI与病人预后关系,并评估二者的联合预测价值是否优于单独预测价值。现作报道。
HTML
-
选取2011年1月至2012年2月在我院术前病理诊断为结直肠癌且接受结直肠癌根治术的病人116例。所有病人资料齐全,术前均未接受放化疗,术前7 d常规完成胸片、腹盆腔CT、肠镜等常规检查。其中男60例,女56例;年龄19~85岁,其中>60岁62例,≤60岁54例;病理学组织学分型:高分化29例,中低分化87例。肿瘤分期参照美国癌症联合委员会(AJCC)TNM分期手册第7版[6]。116例病人中位随访时间为40.0个月(6~72个月)。本研究通过了我院伦理委员会的批准,纳入受试者及其监护人均签署知情同意书。
-
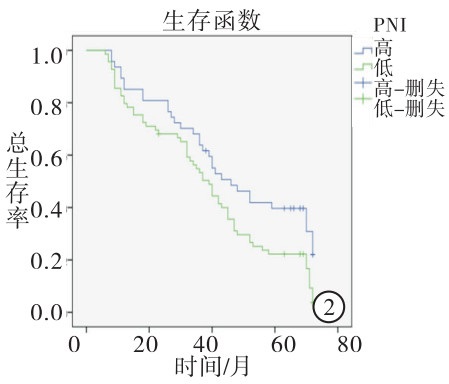
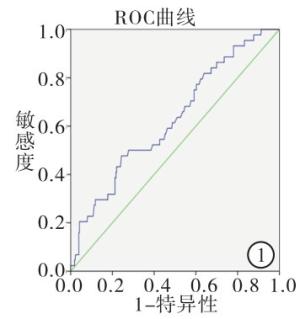
分析包括年龄、性别、肿瘤位置、肿瘤浸润深度、淋巴结转移数目、远处转移、临床分期等病人基本资料,同时调查分析病人入院后的PNI及BMI。术前营养状况评估所需血细胞计数及生化资料均来自于术前一周的常规实验室检查。PNI=血清白蛋白(g/L)+5×淋巴细胞绝对值(×109)。BMI定义为体质量/kg除以身高的平方/m2。WHO将BMI≤18.5 kg/m2认定为体质量过轻,因此,本研究将BMI分为2组:>18.5 kg/m2组(高BMI组)和≤18.5 kg/m2组(低BMI组)。根据病人术后5年生存结局指标绘制用PNI行预后评估的受试者工作特征曲线(ROC)曲线,选取约登指数最大时的PNI值为截断值。根据上述计算的截断值将本组病人分为高PNI组(术前PNI值>截断值)和低PNI组(术前PNI值≤截断值)。为了分析PNI和BMI的联合预测价值,我们将116例结直肠癌病人分为4组:A组为高PNI和高BMI组19例,B组为高PNI组和低BMI组28例, C组为低PNI和高BMI组34例,D组为低PNI和低BMI组35例。
-
采用χ2检验或Fisher′s确切概率法,采用生存分析(Kaplan-Meier法和Cox多因素回归模型)及log-rank检验生存曲线间的差异。
1.1. 研究对象
1.2. 研究方法
1.3. 统计学方法
-
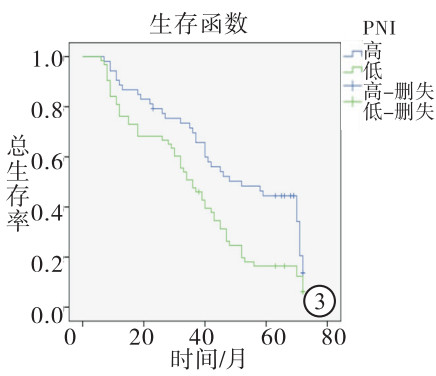
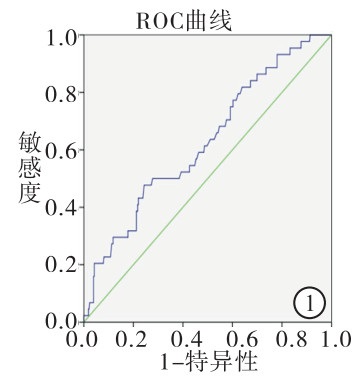
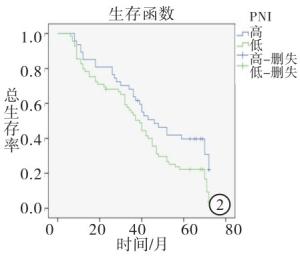
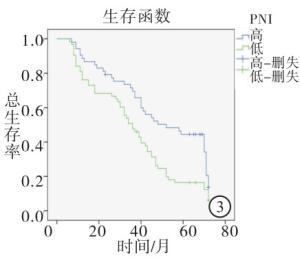
根据病人术后5年生存结局使用ROC曲线选取敏感性和特异性均较高的PNI值为截断值,PNI的截断值为47.5(约登指数为1.133)(见图 1)。47例高PNI组5年生存率40.4%高于69例低PNI组的5年生存率21.7%(χ2=4.712,P<0.05)(见图 2)。BMI>18.5 kg/m2病人53例,5年生存率43.4%,BMI≤18.5 kg/m2病人63例,5年生存率15.9%。高BMI组5年生存率高于比低BMI组的5年生存率(χ2=10.71,P<0.01)(见图 3)。
-
Kaplan-Meier法分析结果提示,PNI和BMI影响结直肠癌预后。高PNI组中位生存时间为46.00个月(95% CI:32.94~59.06),大于低PNI组中位生存时间39.00个月(95% CI:32.99~45.01)(χ2=5.72,P<0.05)(见图 2)。高BMI组中位生存时间为52.00个月(95% CI:32.09~71.09.00),高于低BMI组平均生存时间36.00 d(95% CI:29.26~49.74)(χ2=8.01,P<0.01)(见图 3)。将病人性别、年龄、肿瘤位置、肿瘤分化程度、浸润深度、淋巴结转移、远处转移、临床分期、PNI和BMI进行单因素多重变量的Cox等比例风险模型分析,结果表明肿瘤分化、浸润深度、淋巴结转移、远处转移、临床分期、PNI和BMI对病人预后有意义(P<0.05~P<0.01)。将单因素分析有意义的变量纳入多因素分析,结果表明肿瘤分化、远处转移、临床分期、PNI、BMI等与病人预后有关系(P<0.05),其中低PNI病人死亡风险是高PNI病人死亡风险的1.752倍(95%CI:1.131~2.713)(P<0.05),低BMI病人死亡风险是高病人死亡风险的1.620倍(95%CI:1.052~2.495)(P<0.05)(见表 1)。
自变量 单因素分析结果 多因素分析结果 HR 95% CI χ2 P HR 95% CI χ2 P 年龄 1.144 0.762~1.716 0.42 >0.05 — — — — 性别 1.192 0.796~1.783 0.73 >0.05 — — — — 肿瘤位置 1.231 0.946~1.601 2.41 >0.05 — — — — 分化程度 0.428 0.259~0.705 12.72 <0.01 0.575 0.335~0.989 3.99 <0.05 浸润深度 1.343 1.086~1.661 7.76 <0.01 — — — — 淋巴结转移 1.280 1.001~1.635 3.36 <0.05 — — — — 远处转移 57.166 5.184~630.661 5.71 <0.01 21.015 1.827~241.723 5.97 <0.05 临床分期 1.605 1.243~2.072 13.55 <0.01 1.349 1.025~1.776 4.55 <0.05 脉管侵犯 0.750 0.467~1.206 1.34 >0.05 — — — — 神经侵犯 0.629 0.370~1.070 2.66 >0.05 — — — — PNI 1.648 1.075~2.526 5.49 <0.05 1.752 1.131~2.713 6.32 <0.05 BMI 1.774 1.173~2.684 7.56 <0.01 1.620 1.052~2.495 4.79 <0.05 -
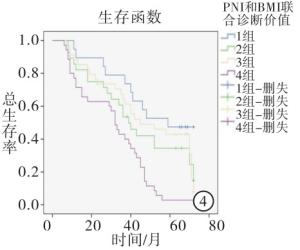
PNI和BMI联合预测价值D组与第A、B、C组比较,均具有较低的1、3、5年生存率(P<0.01)(见表 2)。低PNI且低BMI病人预示着更差的预后,因此PNI和BMI联合预测结直肠癌预后相较于单独作用更加精确(见图 4)。
分组 n 1年生存 3年生存 5年生存 A组 19 19(100.0) 14(73.7) 9 (47.4) B组 28 27(96.4) 18(64.3) 8(28.3) C组 34 34(100.0) 23(67.6) 13(38.2) D组 35 28(80.0)** △△## 15(42.9)**△△## 0(0.0)**△△## 合计 116 109(94.0) 70(60.3) 30(25.9) χ2 — 13.37 6.83 19.62 P — 0.003 0.078 <0.01 χ2分割检验:与A组比较**P<0.01;与B组比较△△P<0.01;与C组比较##P<0.01
2.1. PNI与PNI界点划分
2.2. PNI、BMI与病人预后关系分析
2.3. PNI和BMI联合预测价值
-
PNI和BMI数值仅需通过住院病人的常规血液检查或简单测量即可得到,经济方便,不增加病人负担,是临床常用的免疫营养状况评价指标。同时结直癌预后与代谢、内分泌、免疫、营养等多方面因素密切相关。因此PNI和BMI作为免疫营养状态的评价指数,可能与结直肠癌预后相关[7-8]。本研究探讨了PNI和BMI在结直肠癌病人术后预后中的评估价值,结果显示术前PNI、BMI与病人术后预后相关,提示二者在预测结直肠癌病人术后预后方面具有一定的临床价值。
PNI作为免疫营养状况的有效判断指标,由血清白蛋白和淋巴细胞的绝对值计算而来,最初由日本学者建立,用来评估外科营养状况、预测手术风险及并发症发生率。近年来有研究表明PNI与炎症、多种肿瘤预后相关,尤其是胰腺炎、消化道肿瘤如胃癌、肝癌、结直肠癌等[9-15]。当白蛋白<25 g/L时,提示急性胰腺炎病人预后较差。淋巴细胞绝对值的降低与许多疾病严重程度有关,甚至是一些疾病的独立预后因素。白蛋白的降低或淋巴细胞绝对值的减少,预示着许多疾病预后不良。CAO等[15]研究表明,PNI<44.55时,结直肠癌病人术后发生感染、吻合口瘘等并发症机率增加,同时预示着5年生存率较低。本研究表明高PNI病人较低PNI病人远期生存率更高,与国内外研究结果相一致。但低PNI结直肠癌病人预后较差的机制目前仍不十分清楚,可能是营养不良与病人免疫抑制相关[16-17]。同时淋巴细胞是机体免疫系统的重要组份,在机体抵抗肿瘤过程中发挥着重要作用, 淋巴细胞绝对值的减少意味着抗肿瘤能力降低[18]。
BMI是另一个能够判断病人免疫营养状况的有效指标,低BMI(≤18.5 kg/m2)常预示着免疫抑制。既往研究表明与胃肠道肿瘤术后并发症发生风险,但近年来越来越多的证据表明BMI与肿瘤预后相关[7, 19-23]。FERGUSON等[21]一项纳入1 369例肺癌病人的回顾性研究表明,低BMI肺癌病人具有更高的并发症发生率和死亡率。同时,有研究表明食管癌病人中高BMI高的病人术后并发症较多,但生存期明显延长[7]。SMITH等[22-23]研究表明,BMI与食管癌分期和分化有关。目前BMI与结直肠癌的预后关系国内外研究较少。本研究生存分析结果表明高BMI组比低BMI组5年生存率更高,提示BMI可能与结直肠癌病人预后存在相关性。
虽然越来越多证据表明,PNI和BMI与肿瘤病人预后相关,但其预测的准确性仍存在争议。SONG等研究表明PNI能够预测病人预后,但相对NLR预测准确性较差[24]。ITOH等[25-26]对BMI预测肝癌预后的准确性也存在异议[25-26]。EJAZ等[27]使用血清白蛋白水平联合BMI预测模型提高了BMI预测胃癌预后的准确性。结果表明,本研究中低PNI且低BMI组病人较其他各组相比预后更差,差异有统计学意义。PNI和BMI联合评估结直肠癌病人的预后,增加了判断的准确率。
综上所述,PNI、BMI与结直肠癌病人预后存在相关性并且经济方便,可能成为预测结直肠癌病人预后的临床标志物,适宜在临床上广泛推广。同时,PNI和BMI联合评估预后能够提高准确性,有望将联合评估模型用于评估病人预后,从而在术前制定相应的营养及辅助治疗策略。同时,本研究样也存在一定局限性。研究样本量较小,研究模型仍需更大规模的临床研究验证;PNI在现有研究中的截断值各有不同,仍需大样本的研究来探索统一的标准;PNI与BMI预测病人预后的机制尚需进一步的研究。






 DownLoad:
DownLoad: