-
心尖肥厚型心肌病(apical hypertrophic cardiomyopathy, AHCM)是肥厚型心肌病的一种特殊类型,有研究[1]显示,AHCM老年病人心房颤动、脑卒中、慢性心力衰竭等心血管事件的发生率及死亡率均明显增高[1]。早期心尖肥厚型心肌病(pre-apical hypertrophic cardiomyopathy, PAHCM)病人常因临床症状不明显或较轻,极易被漏诊。因此,提高PAHCM的诊断率对临床及早预防心血管事件具有一定意义[2]。本研究分析32例PAHCM病人超声心动图及声学造影资料,并与健康志愿者作比较,总结PAHCM的超声特征,旨在提高本病的诊断准确率。现作报道。
HTML
-
选取2016-2017年我院就诊疑似肥厚型心肌病的病人60例,入选标准:具有肥厚型心肌病家族史且心电图检查出现异常。所有病人均行超声心动图、心脏声学造影、磁共振成像(MRI)和标准12导联心动图检查。以MRI为金标准[3],共有32例病人确诊为PAHCM,作为PAHCM组。诊断标准:病变部位局限于左室乳头肌水平以下的心尖部,呈弥漫性或局部节段性心肌肥厚,舒张末期心尖部心肌厚≥11 mm且<15 mm,舒张末期心尖部心肌的最大厚度与左室后壁心肌厚度比值≥1.3[4],排除高血压、心脏瓣膜病变、运动员生理性等其他心源性或系统性原因引起的心肌肥厚[5-6]。同期选取32名健康志愿者作为正常对照组,入选标准:体检无心血管系统阳性体征,无冠心病、高血压、瓣膜病、先天性心脏病、心律失常、超声心动图、心电图和胸部X线片检查均未见异常。
-
采用Philips EPIQ 7C型超声诊断仪,S5-1超声探头,频率1~5 MHz,帧频55~90帧/秒。造影剂选用的是意大利Bracco公司生产的SonoVue,使用时先用5 mL 0.9%氯化钠注射液稀释,手工震荡20 s后变成乳白色的微泡混悬液。在肘部正中静脉处建立静脉通道,抽取2.5 mL混悬液,以0.9 mL/min的速度推注至静脉通道内,最后再用5 mL 0.9%氯化钠注射液以相同速度冲管。
-
常规连接心电图实时监测心率,嘱受检者左侧卧位,常规超声心动图检测并记录4个心动周期的胸骨旁左室长轴切面、二尖瓣水平、乳头肌水平及心尖短轴切面,心尖四腔、两腔及三腔切面。设置声学造影模式,将超声诊断仪的机械指数设置为0.08,心动周期设置为20,在静息状态下点击动态采图,分别记录下心尖四腔、三腔及两腔切面在“flash”闪烁前5个左右的心动周期及闪烁后15个左右的心动周期。所有图像均由专人录制,保证图像的质量及稳定性。
-
于声学造影条件下,待造影剂均匀充盈左室腔,心内膜界限显影清晰时,测量舒张末期左室心尖部心肌的最大厚度(AT)、舒张末期左室后壁心肌厚度(LVPWT)、计算得出舒张末期左室心尖部与后壁心肌厚度比值(AT/LVPWT)、Simpson′s法测得左室射血分数(LVEF)。于常规超声心动图条件下,测量左室心肌重量(LVM)、双平面面积长度法测量收缩末期左房容积(LAV)、四腔心切面测量舒张期二尖瓣血流频谱E峰与A峰的比值(E/A)。应用QLab10.0软件中的ROI插件对声学造影条件下的心尖四腔、两腔及三腔切面进行分析,通过函数公式对造影结果进行曲线拟合得出相应节段的时间-强度曲线,并获得该心肌节段心肌灌注指标:造影剂平台峰值强度(A)、曲线上升的斜率(β)、并计算A×β值。上述所有数值均测量3次,取平均值。
-
左室心肌节段按照美国超声心动图协会推荐的17节段分法。将PAHCM组分为2个亚组:P-AM组代表PAHCM病人心尖部肥厚的心肌节段,共92个节段;P-LVPW组代表PAHCM病人左室后壁心肌节段,共64个节段。正常对照组也分为2个亚组:N-AM组代表心尖部心肌节段,共160个;N-LVPW组代表左室后壁心肌节段,共64个。
-
采用t检验和χ2检验。
1.1. 研究对象
1.2. 仪器与方法
1.2.1. 超声仪器和造影剂
1.2.2. 超声图像采集
1.2.3. 超声图像分析
1.2.4. 心肌分组
1.3. 统计学方法
-
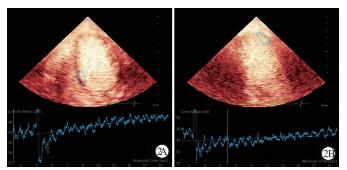
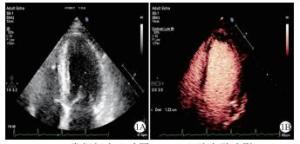
60例疑似肥厚型心肌病的病人经MRI检查,32例确诊为PAHCM。该60例受检者在单独使用常规超声心动图检查时,仅14例被诊断为PAHCM,以MRI为金标准,常规超声心动图的真阳性9例,假阳性5例,敏感性28.1%,特异性82.1%。该60例受检者在使用心脏声学造影检查时,32例被诊断出PAHCM,以MRI为金标准,假阳性为0,敏感性100%,特异性100%(见图 1)。PAHCM组心电图检查均出现为ST-T改变,主要表现为T波倒置、ST段水平型下移、左室高电压。2组在性别、年龄、身高和体质量方面差异均无统计学意义(P>0.05)(见表 1)。
分组 n 男 女 年龄/岁 身高/cm 体质量/kg 正常对照组 32 22 10 46.41±12.53 168.56±6.46 63.81±7.85 PAHCM组 32 21 11 48.25±11.47 168.77±6.33 65.62±8.15 t — 0.07* 0.61 0.13 0.91 P — >0.05 >0.05 >0.05 >0.05 *示χ2值 -
与正常对照组比较,PAHCM组的AT/LVPWT、LAV、LVM指标均增高(P<0.05),AT明显增高(P<0.01),E/A比值明显下降(P<0.01);2组LVPWT、LVEF差异无统计学意义(P>0.05)(见表 2)。
分组 AT/mm LVPWT/mm AT/LVPWT LAV/mL LVM/g LVEF/% E/A 正常对照组 8.24±1.21 9.03±0.76 0.95±1.04 41.25±8.57 116.35±24.51 68.45±4.67 1.23±0.52 PAHCM组 12.45±1.87 9.12±0.85 1.55±1.15 45.76±9.06 131.01±21.31 66.79±6.32 0.69±0.41 t 10.69 0.45 2.18 2.07 2.55 1.20 4.61 P <0.01 >0.05 <0.05 <0.05 <0.05 >0.05 <0.01 -
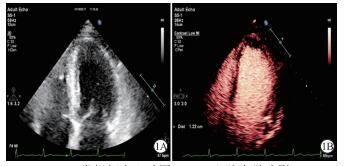
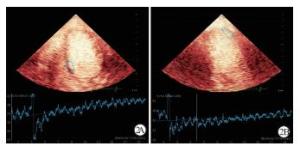
与N-AM组比较,P-AM组A、β及A×β值均明显下降(P<0.01);与P-LVPW组比较,P-AM组A值下降(P<0.05),β及A×β值明显下降(P<0.01)(见图 2);与N-LVPW组比较,P-LVPW组的A、β及A×β值变化差异均无统计学意义(P>0.05)(见表 3)。
分组 n A/dB β/s A×β/(dB/s) P-AM组 92 6.86±1.74 0.81±0.43 5.89±2.64 N-AM组 160 7.50±1.65 1.18±0.49 8.17±3.11 t — 2.91 6.03 5.91 P — <0.01 <0.01 <0.01 P-LVPW组 64 7.48±1.59* 1.15±0.67** 7.93±2.69** N-LVPW组 64 7.51±1.71 1.17±0.36 8.15±2.92 t — 0.10 0.21 0.44 P — >0.05 >0.05 >0.05 与P-AM组比较*P<0.05,**P<0.01
2.1. 2组一般情况比较
2.2. 心脏构型及心功能指标的比较
2.3. 心肌声学造影指标的比较
-
AHCM作为肥厚型心肌病的一种亚型,被认为是常染色体显性遗传性疾病,以男性多见[7]。PAHCM作为AHCM的早期阶段,随着时间推移,可能会发展为典型的AHCM。超声心动图因经济实惠、便捷、无创、无辐射等特点,被认为是目前筛查此类疾病高危人群的首选检查方法。本研究通过对32例PAHCM病人的超声心动图及声学造影资料进行分析,并与正常对照组比较,旨在总结PAHCM超声特征,提高诊断准确率。
为了避免因体表面积不同在心脏构型指标的比较中产生误差,本研究特意选择身高、体质量等一般情况指标与PAHCM组无明显差异的健康受检者作为正常对照组。PAHCM组常规超声心动图指标AT、AT/LVPWT、LVM、E/A、LAV与正常对照组相比差异有统计学意义。PAHCM病人心尖部心肌肥厚、心肌重量增加,这与病变心肌细胞肥大、心肌纤维粗大排列紊乱、结缔组织增生等因素有关。PAHCM组E/A比值较正常对照组下降,提示左室舒张功能减低。心肌对钙离子的敏感性增强,影响舒张期钙离子解离,阻碍肌动蛋白和肌球蛋白之间横桥分离,心肌松弛速率降低,心肌僵硬度增加,从而引起舒张功能障碍[8-9]。PAHCM组LAV增大,这是因为左室舒张功能减低,左室充盈压增高,左房容积受压力负荷的影响而增大[10-11]。
心脏声学造影包括心肌声学造影和心腔声学造影两部分。心肌声学造影技术是检测心肌血流灌注的新技术,通过公式y(t)=A[1-e-βt]+B拟合获得时间-强度曲线,得出平台峰值强度A、曲线上升的斜率β,A为局部心肌组织蓄积微气泡的数量,反映心肌血容量;β为局部心肌的造影剂充填速度,反映心肌血流速度;二者乘积A×β值,反映局部心肌血流量。P-AM组与P-LVPW组之间相比较,A、β及A×β值差异均有统计学意义;P-AM组与N-AM组相比较,A、β及A×β值差异均有统计学意义,这可能与肥厚心肌微循环受损有关[12]。有研究[13-14]表明,心肌微循环障碍可导致并发心肌缺血、心律失常、心衰,甚至心源性猝死,因此监测PAHCM微循环对临床评估PAHCM的发展及预后有着重要意义。本研究结果表明,A、β及A×β值在P-LVPW组与N-LVPW组之间比较差异均无统计学意义。由此提示,PAHCM病人可通对心尖肥厚心肌与自身左室后壁心肌声学造影指标的比较,及时发现病变心肌微循环灌注减低的情况,并定量评价,为以后随访复查提供参考依据。
PAHCM组中大部分病人无明显临床症状,仅少部分病人有胸闷、气短的表现,但心电图检查均出现ST-T改变,以MRI作为金标准,常规超声心动图对PAHCM检测的敏感性仅28.1%、特异性82.1%,而超声心动图结合声学造影检测的敏感性高达100%、特异性100%。常规超声心动图漏诊原因可能是由于胸部透声条件影响,近场回声较弱,心尖部二维图像显示欠清晰,部分超声医师诊断经验及仪器调节的经验不足,再加之临床症状及心电图表现缺乏特异性,所以造成漏诊、误诊。已有专家达成共识,当静息状态下不能满意获得常规超声心动图图像时,使用超声造影剂将明显提高图像质量、增强判断信心和诊断准确性[15]。由此提示,对于心电图出现异常的病人,尤其是有肥厚型心肌病家族史的病人,即使常规超声心动图未见明显异常,也有行心脏声学造影检查的必要性,为临床明确诊断提供依据。
综上所述,超声心动图结合声学造影,不仅能清晰显示心尖部解剖结构,提高PAHCM的诊断准确率,同时还可定量评价心肌微循环灌注情况,具有较高的临床应用价值,值得推广。






 DownLoad:
DownLoad: