-
骨质疏松性椎体压缩骨折(osteoporotic vertebral compression fracture, OVCF)的发病率逐年增高,我国每年大约有110万OVCF病人[1],50岁以上中老年病人中约有25%受其困扰[2]。对于OVCF的治疗,多数专家及学者建议行手术治疗,包括经皮椎体成形术(percutaneous vertebroplasty, PVP)及经皮椎体后凸成形术(percutaneous kyphoplasty,PKP),其创伤小,恢复快,有效缓解疼痛,可早期下地,有效避免卧床带来的并发症[3-7]。“三明治”型OVCF为一种特殊类型骨折,表现在一节完整的椎体上下邻近椎体均发生了OVCF,我们称之为夹心椎体。当对其上下骨折椎体进行骨水泥强化后,是否会双向增加其应力负荷,导致夹心椎体术后骨折。PITTON等[8]在2008年报道中,纳入11例病人,随访后发现夹心椎体骨折的发生率高达55%,由此引起部分专家及学者的重视。WANG等[9]在2012年通过对42例行PKP治疗的“三明治”型椎体进行随访发现,9例病人出现夹心椎体骨折,骨折率约为21%。由于受到双重压力负荷,导致椎体易于骨折[10]。将夹心椎体进行小剂量(约2mL)骨水泥强化后,在增加椎体本身强度和刚度的同时,可最大限度地减少本身强化带来的椎板变形及偏曲,减少对邻近骨折椎体的应力,并且可以有效避免骨水泥注入过多带来的渗漏及肺栓塞等并发症。笔者收集石家庄市第一医院2015年1月至2018年8月行PKP治疗的“三明治”型OVCF病人共58例,其中29例病人在常规行PKP基础上进行夹心椎体小剂量骨水泥(约2mL)预防性强化,另外29例夹心椎体不强化,随访观察夹心椎体骨折情况,分析“三明治”型OVCF病人行PKP时对夹心椎体进行小剂量骨水泥预防性强化的必要性。
-
58例行PKP治疗的“三明治”型OVCF病人,其中男25例,女33例。所有病人术前常规行X线、CT及MRI检查。其中在常规行骨折椎体PKP治疗基础上进行夹心椎体小剂量骨水泥预防性强化的病人29例(观察组),未对夹心椎体进行强化的病人29例(对照组)。所有病人均获得随访,随访12~36个月。根据随访结果观察夹心椎体是否发生骨折, 并比较术前骨密度、年龄、体质量指数等指标。此临床研究已通过石家庄市第一医院医学伦理委员会审批,所有研究对象术前均自愿签署手术同意书及临床科研知情同意书。
-
纳入标准:(1)OVCF病人;(2)骨折部位疼痛明显,有明显压叩痛,无神经及脊髓损伤表现;(3)影像学可见骨折椎体丢失高度≥1/4,且为新鲜骨折。排除标准:(1)非OVCF病人;(2)骨折部位疼痛不明显,局部无明显压叩痛;(3)陈旧性椎体压缩骨折、爆裂骨折或脊柱转移瘤、血管瘤所致骨折;(4)CT或MRI可见椎体后壁不完整。
-
病人俯卧位,用2%利多卡因行局部浸润麻醉直至骨膜,在C型臂透视下正确定位伤椎及椎弓根后,切开皮肤约0.5cm,行单侧椎弓根穿刺,针尖到达椎体前中1/3处建立工作通道,更换球囊到达椎体,缓慢扩张球囊,恢复椎体部分高度,将骨水泥(3~5mL)缓慢注入骨折椎体(观察组中夹心椎体注入约2mL骨水泥),X线监视下防止出现骨水泥渗漏,待骨水泥硬化后拔出套管,手术结束。所有手术均由我科同一高级职称医生完成,所有手术时间均在15~65min内完成,术中未出现骨水泥渗漏,术后均行伤椎影像学检查。
-
鼓励病人术后6h在腰围保护下适当下地活动,最迟不超过48h,术后3~10d出院,术后常规给予基础抗骨质疏松药物治疗,出院后3、6、12、36个月门诊复查伤椎X线片。
-
通过随访,复查X线片(必要时行MRI检查),观察所有病人夹心椎体发生骨折的情况。
-
采用t检验和χ2检验。
-
2组病人年龄、体质量指数及术前骨密度差异均无统计学意义(P>0.05)(见表 1)。
分组 n 年龄/岁 体质量指数/(kg/m2) 术前骨密度/(g/cm2) 观察组 29 74.1±5.1 22.7±2.0 -2.7±1.5 对照组 29 74.7±5.8 22.0±2.1 -2.9±1.4 t — 0.42 1.30 0.52 P — > 0.05 > 0.05 > 0.05 表 1 2组病人一般资料的比较(x±s)
-
观察组有1例(3.45%)发生夹心椎体骨折,对照组有8例(27.59%)发生邻近椎体骨折,2组椎体骨折发生率差异有统计学意义(χ2=4.73,P < 0.05)。
-
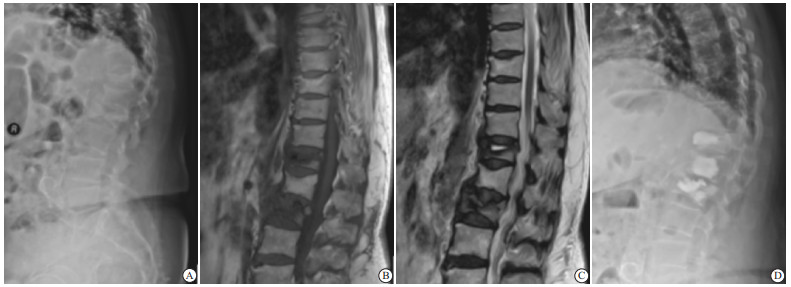
病人,女,78岁,于2016年10月出现T12、L2椎体新鲜压缩骨折,骨折3 d后行T12、L2 PKP治疗,L1预防性注入少量骨水泥,随访至今未发现L1椎体再骨折现象(见图 1)。
-
目前关于PKP术后继发邻椎骨折危险因素的研究较多,年龄、性别、手术方式、穿刺方式、体质量指数、骨密度、骨水泥注射量、骨水泥是否渗漏、后凸畸形等因素[11-21]均有所报道。本研究中选择的2组研究对象的年龄、体质量指数及术前骨密度方面差异均无统计学意义(P>0.05)。本研究中所选研究对象均为老年骨质疏松性骨折病人,术前骨密度均 < -2.5,注射量均 < 5mL,均行单侧椎弓根注射,术中未出现骨水泥渗漏,术后常规进行抗骨质疏松治疗,从而尽量减少相关影响因素。本研究虽未将局部后凸畸形纳入研究,但术中尽量做到使椎体高度得到部分恢复,骨水泥填充均匀,尽量避免因骨水泥分布不均造成的椎体局部弹性模量改变而引起邻椎应力过度集中,从而引起骨折可能。从生物力学角度分析,骨水泥注入骨折椎体后会增加椎体的强度和刚度,改变椎体表面的应力分布,导致相邻椎体的应力也相应发生改变,易发生邻椎骨折。当行PKP后,椎体的高度得到部分恢复,椎体的终板向外膨出与偏曲,从一定程度上亦增加了邻椎的应力。对骨折邻近正常椎体进行骨水泥预防性强化是否合适,一直未有明确的定论。KAYANJA等[22]提出,对OVCF病人进行椎体成形术时,若邻近椎体存在骨折风险,应一并注入骨水泥,可有效预防术后骨折的发生。同样对未发生骨折的椎体进行骨水泥预防性强化可增加椎体的衰竭负荷,在椎体刚度方面要比骨折后再行骨水泥强化更具有优势[23]。EICHLER等[24]通过对单节段OVCF的邻近椎体进行骨水泥预防性强化发现,术后邻椎骨折的风险与未强化组差异无统计学意义。KURUTZ等[25]通过对尸体标本进行生物力学研究发现,对骨折邻近正常椎体进行骨水泥强化有助于减少邻椎骨折的发生。但在临床上如何选择预防性椎体强化至关重要。朱光明等[26]报道,OVCF PKP术后再次经PKP治疗能有效降低疼痛,恢复椎体高度。
骨折椎体骨水泥的注射量是否与邻近椎体骨折的发生有关一直是讨论的焦点。较早报道骨水泥注射量一般为2~15 mL,颈椎平均2.5 mL,胸椎平均5.5 mL,腰椎平均7.0 mL。骨折椎体注射的骨水泥并非越多越好,注射越多,会导致邻近椎体承载的负荷越大,越易发生骨折,骨水泥填充只需要达到椎体的15%(约3.5 mL)即具有较好的临床效果[27]。LIEBSCHNER等[28]通过研究认为,椎体注入约2 mL骨水泥就能将病变椎体的强度恢复到骨折前水平。椎体内注入过度的骨水泥,会使相邻节段椎体的弹性保护丢失,从而失去了有效的力学缓冲保护,相邻节段椎体更容易受到手术椎体刚性变化带来的力学载荷冲击,继而发生骨折[29]。刘仕友等[30]通过重建胸腰段三维有限元模型,模拟L1椎体骨质疏松性压缩性骨折及PKP治疗,并对T12椎体进行不同剂量骨水泥预防性强化,观察不同载荷下邻近椎体的应力,通过研究结果得出以下结论:在2、3、4 mL骨水泥强化时,主要引起T12椎体本身应力的变化,余椎体、椎间盘的最大应力变化幅度均 < 3%, 差异无统计学意义,应力分布无明显变化,故认为对邻近椎体行小剂量的骨水泥预防性强化具有相对安全性。本研究中,将夹心椎体进行小剂量(约2mL)骨水泥强化后,在增加椎体本身强度和刚度的同时,可最大限度地减少本身强化带来的椎板变形及偏曲,减少对邻近骨折椎体的应力。
由于“三明治”型OVCF的特殊性,当对上下骨折椎体均进行骨水泥强化后,夹心椎体将受到上下侧应力的双向叠加,更易发生骨折。当对“夹心椎体”进行骨水泥预防性强化治疗后,椎体本身强度和刚度增加,从而增加了对抗上下强化椎体的应力叠加的能力,防止受到上下强化椎体应力的双向叠加而出现骨折,理论上能降低夹心椎体骨折的发生率。
在手术操作中,应将骨水泥注射均匀,确保骨水泥在椎体内均匀弥散,防止造成应力不均;要严格在X线监视下操作,在拉丝期将骨水泥缓慢注射,防止出现骨水泥渗漏,尽量降低人为因素带来的影响。本研究通过对夹心椎体进行小剂量骨水泥预防性强化,随访发现,观察组术后夹心椎体骨折的发生率(3.45%)明显低于对照组(27.59%),差异有统计学意义(P < 0.05),降低了部分病人行二次手术的概率,减轻了病人的经济负担。
综上所述,对“三明治”型OVCF的夹心椎体进行小剂量的骨水泥预防性强化,在增强夹心椎体刚度和强度的同时,可有效降低术后夹心椎体骨折风险,具有一定的临床意义,但不建议将所有骨折椎体的邻近正常椎体均进行预防性强化。由于本研究样本量较小,随访时间相对较短,且未将后凸畸形、病人的生活条件等因素纳入研究,故仍需大样本试验进行进一步分析行预防性强化的必要性,从而制定出预防椎体成形术后夹心椎体骨折的最佳策略。
夹心椎体小剂量骨水泥预防性强化治疗“三明治”型骨质疏松性椎体压缩骨折的临床分析
Clinical analysis of small-dose bone cement prophylactic strengthening of sandwich vertebra in the treatment of "sandwich" osteoporotic vertebral compression fracture
-
摘要:
目的探讨“三明治”型骨质疏松性椎体压缩骨折(OVCF)行椎体后凸成形术时对夹心椎体进行小剂量骨水泥预防性强化的必要性。 方法选择“三明治”型OVCF行椎体后凸成形术治疗的病人58例,其中观察组29例在常规行骨折椎体后凸成形术基础上进行夹心椎体小剂量骨水泥(约2 mL)预防性强化,对照组29例未行夹心椎体强化,随访观察夹心椎体骨折情况。 结果2组术前骨密度、年龄、体质量指数方面差异无统计学意义(P>0.05);观察组中有1例(3.45%)骨折发生,B组中有8例(27.59%)发生骨折,2组术后骨折率差异有统计学意义(χ2=4.73,P < 0.05)。 结论在常规对“三明治”型OVCF行椎体后凸成形术时,行夹心椎体小剂量骨水泥预防性强化能降低术后夹心椎体骨折风险。 Abstract:ObjectiveTo investigate the necessities of the small-dose bone cement prophylactic strengthening of sandwich vertebra in the treatment of "sandwich" osteoporotic vertebral compression fracture during percutaneous kyphoplasty. MethodsA total of 50 "sandwich" osteoporotic vertebral compression fracture patients treated with percutaneous kyphoplasty were selected, 29 cases were treated with the small-dose bone cement prophylactic strengthening of sandwich vertebra based on the conventional percutaneous kyphoplasty(observation group) and 20 cases were treated without sandwich vertebrula strengthening(control group).The incidence of sandwich vertebral fractures was followed up. ResultsThe differences of the preoperative bone mineral density, age and body mass index were not statistically significant between two groups(P>0.05).One case with fracture in the observation group and 8 cases with fractures in the control group were identified, and the difference of postoperative fracture rate between two groups was statistically significant(χ2=4.73, P < 0.05). ConclusionsIn the conventional percutaneous kyphoplasty of "sandwich" osteoporotic vertebral compression fracture, the small-dose bone cement prophylactic strengthening of sandwich vertebra can reduce the risk of postoperative sandwich vertebral fractures. -
表 1 2组病人一般资料的比较(x±s)
分组 n 年龄/岁 体质量指数/(kg/m2) 术前骨密度/(g/cm2) 观察组 29 74.1±5.1 22.7±2.0 -2.7±1.5 对照组 29 74.7±5.8 22.0±2.1 -2.9±1.4 t — 0.42 1.30 0.52 P — > 0.05 > 0.05 > 0.05 -
[1] SI L, WINZENBERG TM, CHEN MS, et al. Projection of osteoporosis-relatedfractures and costs in China: 2010-2050[J]. Osteoporos Int, 2015, 26(7): 1929. doi: 10.1007/s00198-015-3093-2 [2] SUN ZY, LI XF, ZHAO H, et al. Percutaneous balloon kyphoplasty in treatment of painful osteoporotic occult vertebral fracture: a retrospective study of 89 cases[J]. Med Sci Monit, 2017, 23: 1682. doi: 10.12659/MSM.903997 [3] CHEN D, AN ZQ, SONG S, et al. Percutaneous vertebroplasty comparedwith conservative treatment in patients with chronic painful osteoporotic spinal fractures[J]. J Clin Neurosci, 2014, 21(3): 473. doi: 10.1016/j.jocn.2013.05.017 [4] MARTIKOS K, GREGGI T, FALDINI C, et al. Osteoporotic thoracolumbar compression fractures: long-term retrospective comparison between vertebroplasty and conservative treatment[J]. Eur Spine J, 2018, 27(Suppl 2): 244. [5] CLARK W, BIRD P, GONSKI P, et al. Safetyandefficacy of vertebroplasty for acute painful osteoporotic fractures(VAPOUR): a multicentre, randomised, double-blind, placebo-controlled trial[J]. Lancet, 2016, 388(10052): 1408. doi: 10.1016/S0140-6736(16)31341-1 [6] YUAN WH, HSU HC, LAI KL. Vertebroplasty and balloon kyphoplasty versus conservative treatment for osteoporotic vertebral compression fractures: a meta-analysis[J]. Medicine(Baltimore), 2016, 95(31): 4491. [7] PETERSEN A, HARTWIG E, KOCH EM, et al. Clinicalcomparison ofpostoperativeresultsof balloon kyphoplasty(BKP) versus radiofrequency-targeted vertebral augmentation(RF-TVA): a prospectiveclinical study[J]. Eur J Orthop Surg Traumatol, 2016, 26(1): 67. doi: 10.1007/s00590-015-1711-5 [8] PITTON MB, HERBER S, BLETZ C, et al. CT-guided vertebroplasty in osteoporotic vertebral fractures: incidence of secondary fractures and impact of intradiscal cement leakages during follow-up[J]. Eur Radiol, 2008, 18(1): 43. doi: 10.1007/s00330-007-0694-y [9] WANG L, YANG H, SHI Y, et al. Sandwich vertebral fracture in the study of adjacent-level fracture after vertebral cement augmentation[J]. Orthopedics, 2012, 35(8): 1225. [10] HAN S, JANG IT. Analysis of adjacent fractures after two-level percutaneous vertebroplasty: is the intervening vertebral body prone to re-fracture[J]. Asian Spine J, 2018, 12(3): 524. doi: 10.4184/asj.2018.12.3.524 [11] 黄天霁, 寇玉辉, 殷晓峰, 等. 椎体强化术后再发椎体骨折的临床特点和危险因素[J]. 北京大学学报(医学版), 2015, 47(2): 237. doi: 10.3969/j.issn.1671-167X.2015.02.009 [12] ZHONG BY, WU CG, HE SC, et al. ANVCFV Score System: Assessment for probability of new vertebral compression fractures after percutaneous vertebroplasty in patients with vertebral compression fractures[J]. Pain Physician, 2015, 18(6): 1047. [13] ZHONG BY, HE SC, ZHU HD, et al. Risk prediction of new adjacent vertebral fractures after PVP for patients with vertebral compression fractures: development of a prediction model[J]. Cardiovasc Intervent Radiol, 2017, 40(2): 277. doi: 10.1007/s00270-016-1492-1 [14] LEE DG, PARK CK, PARK, CJ, et al. Analysis of risk factors causing new symptomatic vertebral compression fractures after percutaneous vertebroplasty for painful osteoporotic vertebral compression fractures: a 4-years follow-up[J]. J Spinal Disord Tech, 2015, 28(10): 578. doi: 10.1097/BSD.0000000000000043 [15] LI H, YANG DL, MA L, et al. Risk factors associated with adjacent vertebral compression fractures following percutaneous vertebroplasty after menopause: a retrospective study[J]. Med Sci Monit, 2017, 23: 5271. doi: 10.12659/MSM.907364 [16] HSIAO PC, CHEN TJ, LI CY, et al. Risk factors and incidence of repeat osteoporotic fractures among the elderly in Taiwan: a population-based cohort study[J]. Medicine, 2015, 94(7): 532. doi: 10.1097/MD.0000000000000532 [17] 李晓华, 刘永强, 范金鹏. 椎体成形术后继发邻近椎体压缩骨折相关因素的研究进展[J]. 医学综述, 2019, 25(5): 967. doi: 10.3969/j.issn.1006-2084.2019.05.025 [18] TAKAHARA K, KAMIMURA M, MORIYA H, et al. Risk factors of adjacent vertebral collapse after percutaneous vertebroplasty for osteoporotic vertebral fracture in postmenopausal women[J]. BMC Musculoskelet Disord, 2016, 17: 12. doi: 10.1186/s12891-016-0887-0 [19] YANG S, LIU Y, YANG H, et al. Risk factorsand correlationofsecondary adjacent vertebral compression fracture in percutaneous kyphoplasty[J]. Int J Surg, 2016, 36: 138. doi: 10.1016/j.ijsu.2016.10.030 [20] LIN D, HAO J, LI L, et al. Effect of bone cement volume fraction on adjacent vertebral fractures after unilateral percutaneous kyphoplasty[J]. Clin Spine Surg, 2017, 30(3): 270. doi: 10.1097/BSD.0000000000000204 [21] BORENSZTEIN M, CAMINO WILLHUBER GO, POSADAS MARTINEZ ML, et al. Analysisof risk factors for newvertebral fractureafterpercutaneousvertebroplasty[J]. Global Spine J, 2018, 8(5): 446. doi: 10.1177/2192568217732988 [22] KAYANJA MM, SCHLENK R, TOGAWA D, et al. The biomechanics of 1, 2, and 3 levels of vertebral augmentation with polymethylmethacrylate in multilevel spinal segments[J]. Spine, 2006, 31(7): 769. doi: 10.1097/01.brs.0000207466.40955.31 [23] FURTADO N, OAKLAND RJ, WILCOX RK, et al. A biomechanical investigation of vertebroplasty in osteoporotic compression fractures and in prophylactic vertebral reinforcement[J]. Spine(Phila Pa 1976), 2007, 32(17): 480. doi: 10.1097/BRS.0b013e31811ea2ee [24] EICHLER MC, SPROSS C, EWERS A, et al. Prophylactic adjacent-segment vertebroplasty following kyphoplasty for a single osteoporotic vertebral fracture and the risk of adjacent fractures: a retrospective study and clinical experience[J]. J Neurosurg Spine, 2016, 25(4): 528. doi: 10.3171/2016.2.SPINE15907 [25] KURUTZ M, VARGA P, JAKAB G. Prophylactic vertebroplasty versus kyphoplasty in osteoporosis: A comprehensive biomechanical matched-pair study by in vitro compressive testing[J]. Med Eng Phys, 2019, 65: 46. doi: 10.1016/j.medengphy.2019.01.004 [26] 朱光明, 刘宏鸣, 罗卫华, 等. PKP治疗骨质疏松性椎体压缩骨折术后邻近骨折的临床效果[J]. 蚌埠医学院学报, 2019, 44(12): 1598. [27] ZHANG L, YANG G, WU L, et al. The biomechanical effects of osteoporosis vertebral augmentation with cancellous bone granules or bone cement on treated and adjacent non-treated vertebral bodies: a finite element evaluation[J]. Clin Biomech(Bristol, Avon), 2010, 25(2): 166. doi: 10.1016/j.clinbiomech.2009.10.006 [28] LIEBSCHNER MA, ROSENBERG WS, KEAVENY TM. Effects of bone cement volume and distribution on vertebral stiffness after vertebroplasty[J]. Spine(Phila Pa 1976), 2001, 26(14): 1547. doi: 10.1097/00007632-200107150-00009 [29] 玄文虎, 欧阳剑锋, 王素伟, 等. 小剂量骨水泥椎体后凸成形联合唑来膦酸治疗骨质疏松椎体压缩性骨折[J]. 中国组织工程研究, 2017, 21(26): 4101. doi: 10.3969/j.issn.2095-4344.2017.26.001 [30] 刘仕友, 路青林, 郑伟, 等. 椎体后凸成形椎间盘骨水泥渗漏时行相邻椎体预防性强化的有限元分析[J]. 中国组织工程研究, 2012, 16(22): 4001. doi: 10.3969/j.issn.1673-8225.2012.22.003 -





 下载:
下载: