-
肾脏肿瘤是泌尿外科占第二位的肿瘤,其中绝大部分是恶性的,主要治疗方法是根治切除术。目前, 随着腹腔镜技术的迅猛发展, 腹腔镜肾癌根治术已广泛应用于临床。多数泌尿外科医生习惯经腹膜后腔入路[1],该途径虽然显露肾蒂较容易,但操作空间狭小, 对于右侧病变,术中处理右肾静脉较左侧要复杂,一旦处理不当,极易造成右肾静脉和/或下腔静脉的损伤,严重者可引起大出血,甚至危及生命。我科对右肾肿瘤病人行后腹腔镜下肿瘤根治术时, 在处理右肾静脉将常用方法作了改进,现作报道。
HTML
-
选择2014-2018年收治的右肾肿瘤病人35例, 男23例,女12例,年龄39~76岁。术前经超声、CT(平扫+增强)诊断为右肾肿瘤,肿瘤直径2.5~8.2 cm。临床分期为T1~2N0M0, 术前检查排除右肾静脉及下腔静脉瘤栓, 左侧肾脏ECT检查提示功能正常。肾唇附近离断右肾动脉16例(A组),下腔静脉右侧壁旁离断右肾动脉19例(B组)。
-
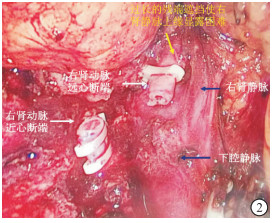
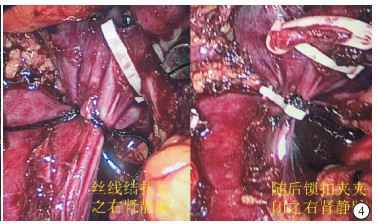
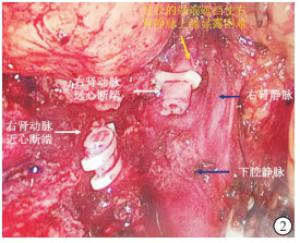
2种手术方法为随机选择,且由同一组手术人员操作完成。采用全麻,取左侧卧位,升高腰桥,常规“三孔法”建立后腹膜腔,二氧化碳气体压力为12 mmHg,超声刀清除部分腹膜外脂肪后,沿腰肌旁纵行切开肾周筋膜后层,上至膈顶,下至肾下极,注意保护腹膜完整性。于肾周筋膜后层与肾脂肪囊间疏松间隙无血管区将右肾顿、锐性游离至肾门处, 根据动脉搏动显露肾动脉及血管鞘,打开血管鞘后将右肾动脉游离。A组:尽量向肾门方向游离右肾动脉至肾唇附近,于此处将右肾动脉主干用3个Hem-lok夹闭并离断,近心断端留2个或3个Hem-lok,远心端1个(见图 1)。B组:向下腔静脉右侧壁旁游离右肾动脉,于此处将右肾动脉主干同法用3个Hem-lok夹闭并离断(见图 2)。然后2组操作均继续游离出右肾静脉用Hem-lok夹闭并离断,继续在脂肪囊外游离肾脏腹侧、上下极(对于肿瘤位于肾脏中、上极者同时切除右肾上腺),最后于髂血管分叉处离断右输尿管,创面止血,腹膜后置橡皮引流管,取出患肾,术毕。
-
采用t检验。
1.1. 一般资料
1.2. 手术方法
1.3. 统计学方法
-
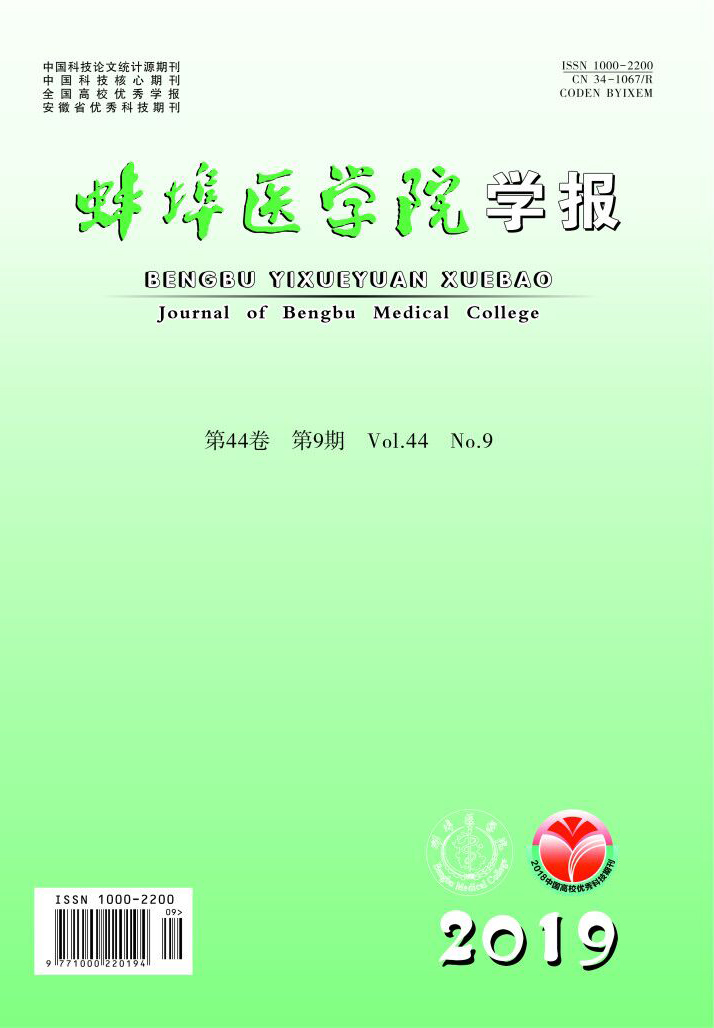
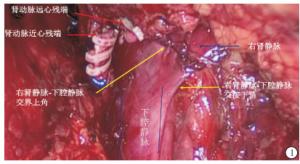
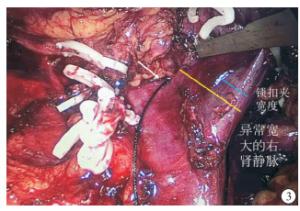
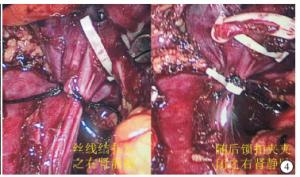
35例手术均在后腹腔镜下顺利完成, 无中转开放手术。术中曾1例右肾静脉超宽病人,其宽度约是规格为2.5 cm×1.0 cm的Hem-lok夹的2倍(见图 3),术中在充分显露右肾静脉汇入下腔静脉两个角后,在腹腔镜下先用丝线结扎使其缩窄后用Hem-lok完全夹闭(见图 4)。
2组各出现3例主操作孔侧小切口延迟愈合,考虑为曲卡引起的皮肤、皮下组织挫伤所致,通过加强换药而恢复,术后4周复查血常规、血生化常规皆无明显异常。A组手术时间、术中出血量及术后拔管时间均少于B组(P < 0.01)(见表 1)。
分组 n 手术时间/min 术中出血量/mL 术后卧床时间/d 术后拔管时间/d 术后住院时间/d A组 16 76.6± 22.5 72.8±9.2 2.6±0.5 2.2±0.6 7.2±0.7 B组 19 116.3±34.6 138.1±8.4 2.2±0.7 5.6±0.8 7.6±0.9 t — 3.94 21.94 1.91 13.99 1.97 P — < 0.01 < 0.01 >0.05 < 0.01 >0.05
-
根治性肾切除是治疗肾肿瘤的有效方法[2-3]。随着微创技术的快速发展, 腹腔镜肾癌根治术越来越被病人所接受,绝大部分肾肿瘤都可以在腹腔镜下完成[4],并成为了治疗T1期肾肿瘤的标准术式[5]。
腹腔镜肾肿瘤根治术根据手术入路可分为经腹腔入路和经后腹腔入路,两种手术方式各有优缺点[6]。经腹腔入路操作空间大,对于肿瘤较大者处理相对容易些[7],但术中需要反复牵拉肠管,既延长了手术时间又干扰了腹腔,还必须在肾静脉后上方处理肾动脉,加大了操作难度[8];经后腹腔入路操作空间相对狭小,对于肥胖、肿瘤较大或瘤体外凸于肾门处的病人处理起来比较困难,但对腹腔干扰小,处理肾动脉相对容易[9-10]。
在经后腹腔入路行肾脏肿瘤根治术时,由于右肾静脉较左肾静脉短,平均长度仅为2.75 cm[11]。有时因为病人肥胖、瘤体较大或瘤体位于肾门部,右肾静脉越发显得短,与左肾手术相比处理起来有时要复杂得多,甚至稍有不慎可能会产生严重的后果,所以在处理右肾静脉时掌握一定的技巧显得尤为重要。
在行后腹腔镜下右肾肿瘤根治切除时,一种常用的方法是:沿着下腔静脉右侧壁游离至右肾动脉从其后面穿出,于此处将右肾动脉主干向远心端游离2~3 cm后用Hem-lok夹闭并离断。此时右肾动脉远心端残段与其前下方之右肾静脉间尚未游离,需继续向远心端游离才能显露出右肾静脉, 而且过长的右肾动脉远心端残段成为处理右肾静脉的一个障碍,往往会遮挡视野使术者处理右肾静脉特别是在游离其上缘时感觉比较困难。我们的体会是:右肾动脉远心端残段往往把其前下方之右肾静脉遮挡,形成“一叶障目”,对于肾门附近脂肪多或瘤体从肾门处凸出者更是明显,使右肾静脉显露变得十分困难,常常会造成右肾静脉和下腔静脉之间解剖不清,在用Hem-lok夹闭右肾静脉时时可能会误伤下腔静脉侧壁或显露困难时用力牵拉会导致右肾静脉汇入下腔静脉处上下角撕裂引起大出血,甚至把下腔静脉误认为右肾静脉进行结扎离断导致非常严重的后果[12]。
本课题组在术中进行了如下改进:根据右肾动脉搏动位置,尽量向肾唇附近游离出2~3 cm右肾动脉主干并离断。此时,在二氧化碳气体压力作用下,右肾动脉远心端残段随着右肾被进一步推向腹内侧,而且其长度又短,所以不易遮挡术野。原来位于其前下方的右肾静脉显露变得容易得多,可以直视下游离出右肾静脉注入下腔静脉处之部分下腔静脉侧壁,清楚地显露出右肾静脉汇入下腔静脉的上下两个角,这样在用Hem-lok夹闭右肾静脉时完全可以避免夹闭不全或误伤下腔静脉。如果右肾静脉与下腔静脉间解剖不清发生夹闭不全,不但可以导致右肾静脉壁穿透,还可以撕裂右肾静脉和下腔静脉夹角,引起大出血,处理起来特别棘手。如果不能做到直视下操作,对少数特殊病例,如右肾静脉过于宽大用常规方法右肾静脉根本无法夹闭,如果盲目夹闭,后果不堪设想。
综上所述,通过改良处理肾蒂血管的方法,使得腹腔镜右肾肿瘤根治术操作变得便利,节省了手术时间,减少了手术创伤,降低了手术风险,提高了手术安全性,此种方法值得借鉴。由于受限于样本量,该改良方法的优劣需更多的临床研究来验证。






 DownLoad:
DownLoad: