-
骨性关节炎属于退行性疾病,包括年龄、劳损、肥胖、创伤、先天性关节异常、关节畸形等众多原因造成的软骨退化损伤以及软骨下骨、关节边缘反应性增生是其发病主要原因[1]。临床表现为进行性关节压痛、疼痛、僵硬、肿胀、功能受限以及关节畸形等,药物治疗虽然一定程度上能缓解疼痛及炎症反应,但大多数学者建议对于退变明显、疼痛严重以及明显关节活动受限的病人应进行手术治疗以达到根治目的[2]。全髋关节置换术(total hip arthroplasty,THA)是治疗骨性关节炎的主要方案,国内外众多临床报道均证实THA在治疗包括骨性关节炎、股骨颈骨折等疾病中具有优良疗效。但值得注意的是,THA虽然能使病人髋功能获得恢复,但术后并发症问题一直是影响THA预后的主要因素[3]。NEWMAN等[4]报道THA病人术后髋关节脱位发生率为4.65%~14.96%,术后髋关节早期脱位已成为THA较为常见的并发症,返修手术对病人造成经济负担及生理痛苦。因此,探寻术后脱位发生的危险因素,对采取针对性措施防治术后脱位具有十分重要的意义。本研究通过分析骨性关节炎THA病人的病历资料,探讨骨性关节炎THA术后脱位发生情况及危险因素,旨在提出针对性预防措施减少THA术后脱位,改善远期预后效果。现作报道。
HTML
-
选择2012年4月至2018年2月于我院治疗的266例骨性关节炎病人,均采用THA治疗,术后随访6个月,记录髋关节脱位发生情况,将术后髋关节脱位病人设为脱位组,未脱位病人设为未脱位组。纳入标准:(1)均符合中华医学会风湿病学分会《骨关节炎诊断及治疗指南》[5]诊断标准;(2)病人同意手术治疗;(3)均顺利完成THA,术后随访6个月;(4)病历资料保存完整;(5)年龄18~80岁,单侧手术。排除标准:(1)先天性下肢发育畸形者;(2)因外伤性骨折等需手术治疗;(3)随访期间遭受严重外伤。
-
THA:常规消毒、铺巾及全身麻醉,术前30 min静滴2.0 g头孢孟多酯钠预防感染。取侧卧位,髋关节后外侧或前外侧做弧形切口,长10~15 mm,逐层切开组织直至髂胫束筋膜显露,纵行切开并进行肌肉组织钝性分离,直至显露后方短外旋肌群,切开肌群,暴露后方髋关节关节囊并做“T”形切开,使关节腔显露。选择股骨小转子上方1.5 mm左右位置,采用摆动锯进行股骨头切除,进行股骨颈成型。髋关节附近滑膜、关节囊进行彻底清理。通过髋臼锉完成髋臼成型,去除髋臼软骨并将软骨下骨组织显露。以前倾20°、外展45°方向安放髋臼假体。随后通过股骨髓腔锉逐步完成股骨髓腔成型,股骨假体试模安放后进行复位,稳定性检查确定髋关节稳定性满意后将髋关节假体试模取出。采用0.9%氯化钠溶液、稀释聚维酮碘反复冲洗后再次安放髋关节假体。术中透视检查明确髋关节假体放置位置良好。再次冲洗后安置1根引流管,逐层缝合关闭切口。术后静脉给予头孢孟多酯钠进行抗感染治疗。髋关节脱位诊断标准[6]:髋关节明显活动性疼痛,关节运动受限,下肢缩短或异常外旋、内旋;经X线检查确诊。影响因素分析:记录2组病人性别、年龄、人工股骨头直径、髋关节手术史、手术入路、合并糖尿病、股骨假体前倾角、股骨偏心距、体质量指数(body mass index,BMI)、手术时间、术后输血率、术后引流量、手术失血量、手术侧别等,分析骨性关节炎THA术后脱位的独立危险因素。
-
采用t检验、χ2检验和logistic回归分析。
1.1. 一般资料
1.2. 方法
1.3. 统计学方法
-
266例骨性关节炎病人THA术后脱位25例,脱位率9.40%,左侧14例(56.00%),右侧11例(44.00%)。
-
2组病人年龄、人工股骨头直径、髋关节手术史、手术失血量、术后股骨假体前倾角、术后股骨偏心距差异有统计学意义(P < 0.05~P < 0.01),而性别、BMI、手术入路、合并糖尿病、手术时间、术后输血率、术后引流量、手术侧别差异无统计学意义(P>0.05)(见表 1)。
项目 脱位组(n=25) 未脱位组(n=241) χ2 P 性别 男 10(40.00) 133(55.19) 2.10 >0.05 女 15(60.00) 108(44.81) 年龄/岁 ≤75>75 16(64.00)9(36.00) 288(78.01)53(21.99) 6.93 <0.01 人工股骨头直径/mm <30 12(48.00) 50(20.75) ≥30 13(52.00) 191(79.25) 9.41 <0.01 髋关节手术史 4(16.00) 12(4.98) 4.87 <0.05 手术入路 前外侧后外侧 7(28.00)18(72.00) 108(44.81)133(55.19) 2.61 >0.05 合并糖尿病 8(32.00) 40(16.60) 3.63 >0.05 BMI/(kg/m2) 22.45±1.87 22.87±1.90 1.05△ >0.05 手术时间/min 57.65±6.56 55.65±6.70 1.42△ >0.05 术后输血率 6(24.00) 54(22.41) 0.03 >0.05 术后引流量/mL 93.66±9.34 95.03±10.02 0.65△ >0.05 手术失血量/mL 323.82±32.77 309.76±29.02 2.28△ <0.05 手术侧别 左 14(56.00) 133(55.19) 0.01 >0.05 右 11(44.00) 108(44.81) 股骨假体前倾角(°) 9.54±1.32 7.96±0.98 7.40△ <0.01 术后股骨偏心距/mm 40.23±3.23 42.65±3.17 3.63△ <0.01 △示t值 -
多因素logistic回归分析结果显示,年龄>75岁、女性、人工股骨头直径<30 mm、髋关节手术史、后外侧入路、术后股骨假体前倾角>10°是骨性关节炎THA术后脱位的独立危险因素(P < 0.05)(见表 2)。
变量 β SE Wald P OR(95%CI) 年龄>75岁 0.834 0.265 8.667 <0.05 2.34(1.12~8.93) 女性 1.322 0.365 9.376 <0.05 2.90(1.41~9.03) 人工股骨头直径<30 mm 1.154 0.360 8.187 <0.05 2.70(1.14~989) 髋关节手术史 1.336 0.375 11.288 <0.05 3.57(1.49~12.32) 后外侧入路 0.956 0.297 7.518 <0.05 2.30(1.20~7.67) 术后股骨假体前倾角>10° 0.855 0.310 6.754 <0.05 2.12(1.27~7.18) -
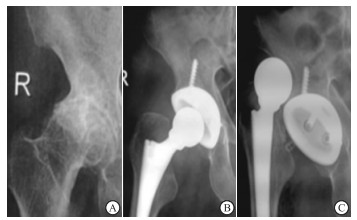
男性,77岁,图 1A正位X线片显示右髋臼发育不良、骨性关节炎;图 1B:接受后外侧入路THA治疗1周复查显示内固定良好;术后2月病人髋关节明显活动性疼痛,关节运动受限,下肢左侧外旋,图 1C正位X线显示髋关节脱位。
2.1. 骨性关节炎病人THA术后脱位发生情况
2.2. 骨性关节炎病人THA术后脱位单因素分析
2.3. 骨性关节炎病人THA术后脱位多因素分析
2.4. 典型病例
-
THA在髋关节功能重建中广泛应用,其通过人造髋关节替换病损髋关节达到改善髋关节疼痛症状,恢复髋关节功能的目的,还能防止髋关节畸形出现或加重。THA适应症众多,股骨无菌性坏死、部分髋部骨折以及骨性关节炎等均可采用THA治疗[7]。但随着THA的临床应用,病人基数逐渐增大,术后并发症对手术预后的影响受到骨科医师的极大重视。术后髋关节脱位是THA最常见的并发症之一,需进行再次翻修手术,对病人髋关节功能恢复产生极大影响[8]。因此探寻术后脱位发生的危险因素,对采取针对性措施防治术后脱位具有十分重要的意义。
关于THA术后脱位发生率报道不一,罗肖等[9]报道GardenⅢ、Ⅳ股骨颈移位骨折病人THA术后脱位率9.72%,YOAHIMOTO等[10]报道THA术后脱位率7.67%,既往研究显示THA术后髋关节脱位发生率为4.65%~14.96%。本研究266例骨性关节炎病人THA术后脱位25例,脱位率9.40%,与既往研究结果一致。THA术后脱位原因众多,可归为3个方面,即自身原因、手术相关原因以及假体因素[11]。随着年龄的增加,髋关节周围软组织明显疏松,肌力显著降低,经THA治疗后出现手术区域及附近软组织张力失衡情况,关节稳定性下降,易造成术后髋关节脱位。TAKEGAMI等[12]报道称年龄>75岁病人THA术后早期脱位风险是≤75岁者的2.37倍,与本研究结果相一致。女性被作为OP的独立危险因素之一,其对THA术后脱位的影响主要与髋部骨质疏松有关[13]。雌激素对早期成骨细胞的分化具有促进作用,同时能刺激胶原蛋白合成。女性绝经后雌激素分泌降低,引起破骨细胞活性上升,骨密度下降,骨转化率增加,钙盐沉积受影响,促进骨消融,骨质大量丢失,骨关节骨脆性增加,稳定性下降,增加脱位风险。人工股骨头直径较大时能够提高关节活动度,降低假体摩擦、碰撞,髋关节及四周软组织获得更强的包容性,从而降低脱位风险[14]。YOSHIMOTO等[15]研究显示人工股骨头直径22 mm、28 mm是THA术后脱位危险因素,>30 mm是保护因素,与本研究结果相一致。髋关节手术史多与病人早期骨折有关,李志昌等[16]认为手术后外展肌力下降,肢体长度未完全恢复或者软组织张力降低等均会髋关节结构稳定性造成影响,再进行THA术时容易脱位。李文龙等[17]一项对比试验认为外侧入路手术操作简单、组织暴露清晰、不易造成臀中小肌损伤。但后外侧入路较前外侧入路对四块肌肉、关节韧带结构破坏较大,影响髋关节稳定性,导致术后关节保护较差,造成假体脱位。既往研究显示假体放置位置对THA术后脱位具有明显影响,集中在股骨假体前倾角、股骨偏心距等方面,本研究中术后股骨假体前倾角>10°是THA术后脱位的独立危险因素,与卢仲琳等[18]报道结果一致。其原因在于术后股骨前倾角度的增加会增加关节假体旋转扭曲,关节松动的风险增加,导致假体脱位。
本研究THA术后脱位发生情况及多因素分析显示,年龄>75岁、女性、人工股骨头直径<30 mm、髋关节手术史、后外侧入路、术后股骨假体前倾角>10°是THA术后脱位的独立危险因素,其临床意义在于术前能通过对术后脱位的高危病人采取针对性干预措施以降低脱位风险;同时具有手术相关危险因素者术后需增加随访及复查频率,密切关注手术效果。
综上所述,骨性关节炎THA术后容易发生髋关节脱位,年龄>75岁、女性、人工股骨头直径<30 mm、髋关节手术史、后外侧入路均可增加其脱位风险。本研究不足之处在于纳入病例数少,结果可能存在偏倚,需后期增加样本量进一步研究。






 DownLoad:
DownLoad: