-
脊柱滑脱症是指一个椎体与其相邻的椎体矢状面相对位置发生改变,导致硬膜囊或是神经根受压,而引起的一系列临床症状和病理过程。腰椎滑脱症在脊柱外科领域是一种常见病,大部分病人仅有轻微症状或是无明显感觉异常症状,仅需保守治疗或无需治疗症状便能自行缓解或是减轻,发生率约5%,但是在这5%的病人中,约有20%的病人经非手术治疗方法无效而需手术治疗[1]。后路椎体间植骨融合术是治疗腰椎滑脱症的有效手段。本文就单纯后路复位减压植骨融合内固定术治疗不同年龄段腰椎滑脱症的临床疗效作一比较。
HTML
-
选择2014年12月至2018年1月我院手术治疗的腰椎滑脱症病人40例,年龄26~77岁。腰痛及下肢放射痛、麻木17例,间歇性跛行23例。40例均行腰椎正位、侧位、双斜位和动力位X线检查,并行CT和MRI检查。以55岁为界限,将40例病人分为2组,26~55岁为A组, >55~77岁为B组。A组19例,男11例,女8例,腰椎滑脱部位L3/4处4例,L5/4处8例,L5/S1处7例;B组21例,男10例,女11例,腰椎滑脱部位L3/4处3例,L5/4处10例,L5/S1处8例。2组病人性别和腰椎滑脱部位差异均无统计学意义(χ2=0.12、0.33,P>0.05), 病人病程、术前痛视觉模拟评分(VAS)、JOA评分和术后随访时间差异亦均无统计学意义(P>0.05)(见表 1)。
分组 n 年龄/岁 病程/月 术前
VAS
评分/分术前
JOA
评分/分随访
时间/月A组 19 46.7±8.2 20.1±5.9 6.1±3.1 11.9±5.5 24.1±5.4 B组 21 59.2±9.8 23.9±7.1 5.8±2.9 12.3±6.2 26.9±6.2 t — 4.35 1.83 0.32 0.21 1.52 P — < 0.01 >0.05 >0.05 >0.05 >0.05 -
病人麻醉满意后,取俯卧位于脊柱手术架上,常规消毒铺巾。以病椎为中心做一长约15 cm后正中切口,逐层切开,剥离双侧骶脊肌,至关节突外侧,显露病椎及下位椎体的双侧椎板,放置横突拉钩。将病椎椎管打开并扩大减压,于病椎及下一椎体植入2对椎弓根螺钉,见病椎与下一椎体形成一台阶,后予钉棒固定,利用病椎椎体的椎弓根螺钉行提拉复位病椎椎体,C臂透视见椎体复位良好。后予病椎椎间盘刮除并行植骨融合,拧紧钉棒连接处。清洗切口,充分止血,切口内置一负压引流,逐层缝合切口。所有病人术后常规甘露醇脱水治疗3 d,抗生素治疗24 h,48~72 h拔除引流管。术后第1天被动或主动行直腿抬高运动,避免神经根粘连,拔管后24 h鼓励病人在支架保护下下地活动。术后摄X线片了解伤椎复位和固定情况。
-
术后l、3、6个月复查腰椎正、侧位X线片(6个月后加摄过伸过屈位片),了解融合情况及固定有无滑脱、断钉、移位等情况。
-
采用t(或t′)检验、χ2检验和Fisher′s确切概率法。
1.1. 一般资料
1.2. 手术方法
1.3. 评价指标
1.4. 统计学方法
-
A组病人滑脱复位率高于B组(P < 0.05)。2组手术时间、出血量、术后VAS评分、JOP评分、假关节形成率、硬膜囊损伤率、椎间隙感染率和切口血肿率差异均无统计学意义(P>0.05)(见表 2)。
分组 n 手术时间/min 出血量/mL 术后
VAS
评分/分术后
JOA
评分/分滑脱
复位假关节
形成硬膜囊
损伤椎间隙
感染切口
血肿A组 19 81.5±13.2 168.2±31.3 1.4±1.2 23.5±5.2 18(94.7) 0(0.0) 1(5.3) 0(0.0) 1(5.3) B组 21 89.3±15.1 182.5±38.6 1.3±1.3 24.2±5.9 13(61.9) 1(4.8) 2(9.5) 1(4.8) 1(4.8) t — 1.73 1.28 0.25 0.40 — — — — — P — >0.05 >0.05 >0.05 >0.05 < 0.05* >0.05* >0.05* >0.05* >0.05* *示Fisher′s确切概率法 -
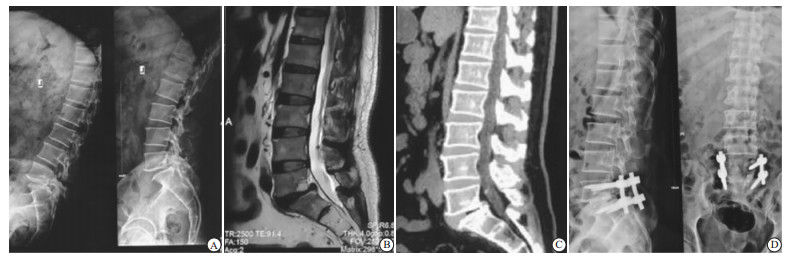
术后X线片均显示椎间高度A组完全恢复,B组不完全复位或是部分复位。B组5例出现下肢麻木、无力,经2个月康复对症治疗消失,考虑术中神经根牵拉所致。2组病人随访6~30个月,腰痛及下肢放射性疼痛症状间歇性跛行均缓解消失。A组植骨均融合,融合器无移动、滑落,无钉棒系统折断等(见图 1、2)。
-
术后2组病人恢复良好,均取得了良好的疗效。2组末次随访VAS评分与JOP评分差异均无统计学意义(P>0.05)(见表 3)。
分组 n VAS评分 JOA评分 A组 19 1.4±1.2 23.5±5.2 B组 21 1.3±1.3 24.2±5.9 t — 0.25 0.39 P — >0.05 >0.05
2.1. 2组病人手术情况比较
2.2. 术后疗效
2.4. 2组末次随访VAS评分、JOP评分情况
-
腰椎滑脱症可见于各类人群,退行性腰椎滑脱以老年人发生率较高,其中男性多于女性,儿童和青年人则以先天性滑脱较为多见。在很长一段时间里认为腰椎后外侧融合术(PLF)是腰椎滑脱手术治疗的主要手段。腰椎滑脱的手术指征最重要的有以下两点:(1)经保守治疗无效,腰部或是下肢症状持续存在;(2)出现明显的神经损害症状,且此种损害对病人生活造成严重影响。腰椎滑脱行手术治疗主要为扩大椎管及神经根管,解除神经受压;恢复腰椎生理弯曲;重建脊柱稳定性。目前临床上认为后路椎体间植骨融合术是治疗腰椎滑脱症的有效手段,借助于椎间融合器可以有效的恢复椎间高度以及神经根管的直径,可有效避免滑脱复位后上位椎体及植骨块的下沉。
减压方法有很多种,临床上常用的有全椎板切除术和椎板间开窗潜行减压等术式,选择减压方式应依照病人的自身情况如临床表现、椎管狭窄程度、椎体滑脱程度及椎间关节退变程度等而定[2]。微创方法经椎旁肌间隙入路治疗腰椎滑脱,可减小手术过程中人为对腰椎后方骨-肌肉-韧带复合体的破坏[3],相较于常规施行的双侧骶脊肌外侧剥离手术,优点在于充分的神经减压和良好的脊柱稳定[4],对腰椎滑脱病人有很好的效果[5-10]。借助于脊柱钉棒内固定系统使滑脱椎体复位,是许多医生追求的目标,此种方法的理论依据是完全的解剖复位是治疗腰椎滑脱所致椎管狭窄的基础。良好的解剖复位可以恢复腰骶段生理弧度,并且进一步改善病人的坐姿和脊柱的外形尤其是下腰段,有利于恢复脊柱的正常生物力学,进而改善病人的生活;同时滑脱椎体的解剖复位增大了椎体间接触面积,为后来的植骨融合提供了有利的外部条件[11-14]。
有学者[15-16]认为65岁以下老年人腰椎滑脱行椎板减压椎间植骨Cage融合钉棒系统内固定术较牢靠,65岁以上老年人腰椎滑脱行腰后路椎板减压后外侧横突间植骨融合较为可行。本文结果显示,26~55岁组病人滑脱复位率高于>55岁组, 手术时间、出血量、术后VAS评分、术后JOP评分、假关节形成率、硬膜囊损伤率、椎间隙感染率和切口血肿率在2组间差异均无统计学意义,末次随访2组VAS评分与JOP评分差异亦均无统计学意义。提示对于病人年龄≤55岁的病人争取把滑脱椎体完全复位,>55岁的病人可不予完全复位,但必须保证神经根松弛,无压迫。






 DownLoad:
DownLoad:
