-
骶骨骨折在脊柱骨折中占比较少,多源于交通事故、高处跌落等高能量损伤,严重的骨骼肌肉损伤多伴有骨盆骨折出现,同时并发神经损伤比例也较高[1],可引起较为严重的并发症,且对手术操作要求较高。髂腰固定是治疗骶骨骨折的主要方案,骶管减压术在解除神经压迫方面具有十分重要的意义[2],但也有学者[3]认为早期骶管减压对远期神经损伤的恢复并无明显作用,这可能与不同研究纳入病例数、骨折分型等有关。为探讨骶骨骨折合并脊柱-骨盆分离的合理治疗方案,本研究回顾性分析创伤性骶骨骨折合并脊柱-骨盆分离病人16例的临床资料,探讨骶管减压联合腰椎-骨盆固定术治疗创伤性骶骨骨折合并脊柱-骨盆分离的临床疗效。现作报道。
HTML
-
选取2012年6月至2016年7月我院收治的创伤性骶骨骨折合并脊柱-骨盆分离病人16例,骨折分型Denis Ⅲ型,均采用骶管减压联合腰椎-骨盆固定术治疗,均随访2年以上。纳入标准:(1)术前经MRI、CT诊断为骶骨Denis Ⅲ型骨折[4],即影像学检查显示通过骶管的骶骨区骨折,并发神经损伤;(2)明确创伤史且合并脊柱-骨盆分离;(3)年龄18~60岁,病人及家属同意手术治疗;(4)无盆骨、脊柱骨折史及手术史;(5)无盆腔器质性病变,无脊柱肿瘤、结核或严重骨质疏松;(6)随访2年以上,病历资料完整。排除标准:(1)骨折线纵向走行;(2)病理性骨折;(3)合并颅内外、心肺等其他组织严重外伤者;(4)病历资料缺失、失访者。其中男10例,女6例;年龄21~58岁;受伤至手术时间4~40 d;受伤原因:交通事故11例,高处跌落5例。合并神经损伤表现为小腿后外侧、大腿后侧、足跟部疼痛症状,合并浅感觉减退,跟腱反射消失,小腿三头肌肌力降低。
-
所有病人均采用气管插管全麻,术前进行X线、MRI、CT等影像学检查,取俯卧位,腰骶手术部位常规消毒铺巾。做常规后正中切口,以骨折具体情况拟定切口范围,通常沿L3~S4方向。沿棘突方向剥离两侧竖棘肌,显露腰椎椎板、横突以及关节突,骶骨显露椎板,沿切口方向将两侧将双侧髂后上棘完全显露。椎弓根螺钉固定位置以脊柱-骨盆分离损伤情况而定,通常选择为损伤平面以上1~2个节段,对应椎体水平置入规格适宜的椎弓根螺钉。双侧髂后上棘作为髂骨螺钉置钉点,以髂后上棘-髂前下棘连接方向将螺钉置入,置入螺钉位置应与髂骨外板平行且位于髂骨内外板间。为避免髂后上棘处内固定物突出造成皮肤压迫,可适当去除螺钉置入点处骨质。预弯连接棒使之符合腰骶部弧度,连接髂骨螺钉以及脊柱椎弓根螺钉。所有病人均进行骶管减压,探查腰骶神经根进并行松解术,或进行骶孔切开、椎板切除等解除神经压迫。减压后采用复位钳、撑开器、Schanz钉手柄等进行复位并安装横联。骨盆前环不稳定者改仰卧位,再次消毒铺巾,采用髂耻螺钉或重建钢板对骨盆前环进行固定。术中透视明确骨折脱位复位且内固定可靠,术毕,采用温0.9%氯化钠溶液对术腔进行反复冲洗并放置引流管,逐层缝合关闭切口。术后48 h进行生命体征监护,定期检查生化指标。术后引流量<50 mL/d时拔出引流管,术后24 h给予抗凝药物预防下肢深静脉血栓,术后3 d采用广谱抗生素预防切口及深部感染。
-
记录病人手术耗时、出血量、住院时间、骨折愈合时间等手术相关指标。术前、末次随访采用Gibbons评分[5]评价神经功能恢复情况:1分,神经功能完全恢复;2分,损伤平面以下残留感觉异常;3分,部分运动障碍但括约肌功能正常;4分,膀胱、直肠、括约肌功能受损。采用Majeed评分[6]评价病人恢复情况及手术疗效:包括疼痛程度、行走、坐、工作、站立等方面,总分为100分,分值越高表明功能恢复越优,>85分、>70~85分、55~70分、 < 55分依此评价为手术疗效优、良、可、差。记录术后并发症情况。
-
采用t检验。
1.1. 一般资料
1.2. 手术方法
1.3. 观察指标
1.4. 统计学方法
-
所有病人均顺利完成手术,手术耗时(172.34±43.23)min,出血量(670.98±98.34)mL,住院时间(25.76±6.45)d,骨折愈合时间(4.21±0.43)个月,随访时间(2.25±0.31)年。
-
病人末次随访时Gibbons评分明显低于术前(P < 0.01),Majeed评分明显高于术前(P < 0.01)(见表 1)。
时间 n Gibbons评分 Majeed评分 术前 16 3.15±0.32 36.45±7.02 末次随访 16 2.03±0.20 81.08±6.45 t — 11.87 18.73 P — <0.01 <0.01 -
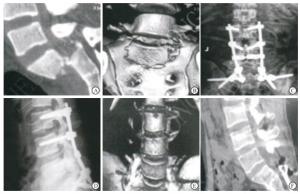
末次随访时,病人根据Majeed评分综合疗效优7例,良4例,可4例,差1例,优良率为68.75%;术后切口感染2例,经清创及万古霉素静脉治疗后控制;褥疮1例,位于髂后上棘,进行清创、负压引流等处理后愈合;均无钢板、连接杆断裂、骨折再移位等严重并发症出现。典型病例见图 1。
2.1. 手术一般情况
2.2. 病人手术前后Gibbons评分和Majeed评分比较
2.3. 手术疗效及术后并发症情况
-
脊柱-骨盆分离在骶骨骨折中约占30%,盆骨骨折中23%~30%存在骶骨损伤。随着近年来骶骨骨折病人基数的增加,骶骨骨折合并脊柱-骨盆分离的治疗逐渐受到骨外科医生的重视,但由于病情复杂,骶骨骨折的诊断及治疗还存在一定争议[7]。骶骨及骶髂关节是机体重量由脊柱过渡到下肢的重要部位,骨盆后环也是承担身体重量重要部位之一,骶髂关节、骶骨是组成后环的重要解剖结构,其稳定性对腰骶部稳定性起到关键作用,因此骶骨骨折合并脊柱-骨盆分离对腰骶部力学连续性及稳定性恢复是临床治疗的主要目标[8]。本研究中Denis Ⅲ型骨折病例多合并神经损伤,髂腰固定术以及骶管减压分别起到恢复局部结构稳定性及解除神经压迫作用,常被用于腰骶结构不稳和神经损伤的病人。
既往对于脊柱-骨盆分离的保守治疗效果较为局限,对于非高龄病人,手术治疗应作为首选治疗方案。腰髂固定系统是常用的脊柱-骨盆固定术,手术将髂骨螺钉以及腰椎椎弓根螺钉置于髂骨及腰椎处,并采用连接棒相连,能够使上身重力经腰髂固定由脊柱向骨盆传导,在恢复腰骶部稳定性的基础上完成力学传导[9]。巩腾等[10]认为该技术具有高效的骨折复位作用,用于骨折分离移位较大者近远期固定效果优良。CHOI等[11]进行生物力学分析显示,腰髂固定系统在三维平面上通过髂骨螺钉、腰椎椎弓根螺钉以及横联装置予以内固定,具有垂直稳定性以及良好的抗旋转作用。同时腰髂固定系统并未对骶骨进行直接固定,从而对于骶骨粉碎性骨折丧失骶髂螺钉通道固定者也可通过脊柱-骶骨部的间接固定促进骨折愈合[12]。但既往该固定技术也有不足之处,例如内固定物对骶尾部及皮肤压迫可能引起褥疮等并发症,本研究通过对髂后上棘钉置入点处骨质进行适当去除,术后病人长期卧床情况下褥疮仅发生3例,有效避免了此方面不足。
目前对于腰骶丛神经损伤的临床治疗仍存在一定争议。既往有研究[13]显示,神经探查、减压无法对脊柱-骨盆分离损伤引起的腰骶丛神经功能起到有效改善作用,同时对于神经根撕裂牵拉伤者,探查减压可能再次损伤受损神经。然而随着CT等影像技术以及手术技术的发展,手术探查、减压逐渐引入临床治疗。一般情况下骶骨翼区骨折经复位后,神经压迫多数情况下能够自行解除,对于中央管内的骨块压迫,采用骶骨椎板全部或部分切除以及骶孔切开也能够解除骨折部位造成的神经压迫,并能有效减少骨痂、瘢痕引发的继发性神经伤害[14]。本研究末次随访时病人手术疗效优良率为68.75%,与黄南翔等[15]研究结果的64.08%相近,同时病人Gibbons评分明显改善,也表明骶管减压联合腰椎-骨盆固定术不仅能够恢复局部结构稳定性,还能解除神经压迫,恢复损伤平面以下的感觉功能。
本研究不足之处在于由于病例数限制以及伦理原则等,未进行随机双盲分组对照试验,待后期条件充足,扩大样本量再作深入研究。综上所述,骶管减压联合腰椎-骨盆固定术治疗能重建创伤性骶骨骨折合并脊柱-骨盆分离病人骨盆环及脊柱稳定性,改善术后神经功能及活动功能。






 DownLoad:
DownLoad: