-
脊柱裂是胎儿发生的神经管畸形之一,在我国的发生率约为0.274%,其中开放性脊柱裂(OSB)占脊柱裂的80%以上。OSB主要的处理方法为尽早选择终止妊娠,以减少对孕妇的身体伤害,因此如何早期筛查OSB具有重要的临床意义[1]。目前,超声检查是OSB主要的筛查方法,但在早孕期由于脊柱骨化未完全,超声难以直接观察脊柱的形态和排列异常等直接征象。近年来有研究[2-4]报道,通过在孕11~13+6周检测胎儿的颅内透明层(IT)超声特征,可帮助诊断OSB,或通过检测胎儿的后脑结构的超声特征,也可筛查OSB。但临床上尚无统一标准,且不同方法间的鉴别效能存在差异,选择合理有效的方法对早期筛查OSB具有重要的作用。本研究回顾性分析OSB胎儿和正常胎儿的颅内特征、IT及后脑结构的超声特征,探讨其在鉴别OSB中的效能,为孕11~13+6周OSB的临床诊断提供依据。现作报道。
HTML
-
选取2011年7月至2017年7月我院收治的OSB胎儿80例作为OSB组,同期选取80名健康胎儿作为健康组。纳入标准:(1)经病史、超声、引产或随访至产后等检查证实是否存在OSB;(2)胎儿母亲20~45岁;(3)孕妇无精神病病史、无沟通交流障碍;(4)孕妇签署知情同意书。排除标准:(1)露脑畸形、无脑儿等胎儿;(2)孕妇有妊娠糖尿病、妊娠高血压等难以控制的疾病;(3)孕妇有心、肝、肾等严重性疾病;(4)拒绝参与本次研究。其中OSB组胎儿男46例,女34例;孕11+6周26例,孕12+6周34例,孕13+6周20例;胎儿母亲年龄20~45岁,体质量指数(BMI)20.97~31.78 kg/m2。健康组胎儿男44名,女36名;孕11+6周28例,孕12+6周30例,孕13+6周22例;胎儿母亲年龄20~45岁,BMI 20.92~31.86 kg/m2。2组胎儿性别、孕周、母亲年龄、母亲BMI等一般资料均具有可比性。本研究经我院伦理委员会审批通过。
-
所有胎儿均在孕11~13+6周给予超声检查间脑及中脑形态,观察IT及后脑结构。胎儿母亲取平卧位,先通过GE Voluson E8型彩色多普勒超声诊断仪(四维经腹部探头和经腔道探头,频率分别为4~8 MHz和6~12 MHz),获得胎儿正中矢状切面,常规检查IT及后脑结构,在胎儿头颅正中矢状切面及横切面上观察并测量颅内透明层厚度(ITT)、脑干直径(BS)、脑干-枕骨间距离(BSOB)(见图 1)。如遇胎儿孕周较小、颅内结构显示不清或孕妇腹壁脂肪厚者,改为经阴道超声观察。上述指标每项测量3次,取平均值,并存图,记录所测量的数据和结果,计算BS/BSOB,采用ROC分析ITT、BS/BSOB及二者联合鉴别OSB的效能,其中二者联合为符合OSB或ITT诊断。
-
采用t(或t′)检验和ROC分析。
1.1. 一般资料
1.2. 方法
1.3. 统计学方法
-
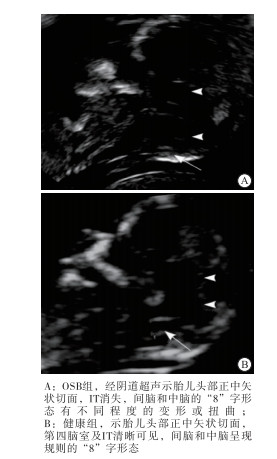
健康组胎儿超声表现为间脑和中脑呈现规则的“8”字形态,IT、BS、小脑延髓池可清晰显示,产后均证实无OSB。
OSB组超声表现为脊柱裂处脊柱横切面“三角形”骨化中心失去正常形态,脑室受压、颅后窝颅内结构移位、IT部分显示受碍,且有不同程度的减小或消失。其中32例可测得ITT,22例显示模糊难以测量ITT,26例显示IT消失,间脑和中脑“8”字形态有不同程度的变形和扭曲,72例裂开处见囊性团块,内可见马尾或脊髓组织,22例和24例分别可见香蕉小脑和柠檬头,30例小脑形态及后颅窝池无明显异常。其中72例在中孕晚期、8例在孕晚期选择行引产术终止妊娠证实为OSB。典型病例见图 2。
-
OSB组ITT、BS、BSOB均明显低于健康组(P < 0.01),BS/BSOB水平明显高于健康组(P < 0.01)(见表 1)。
分组 n ITT/mm BS/mm BSOB/mm BS/BSOB 健康组 80 1.74±0.21 3.01±0.33 4.41±0.47 0.72±0.07 OSB组 80 0.44±0.06 2.43±0.22 2.11±0.32 1.15±0.10 t — 53.24Δ 13.08 36.18 31.51Δ P — < 0.01 < 0.01 < 0.01 < 0.01 Δ示t′值 -
在鉴别OSB方面,ITT以 < 1.0 mm为临界值时,敏感度、特异度分别为90.00%(72/80)、87.50%(70/80),有10例误诊、8例漏诊;BS/BSOB以>1.0为临界值时,敏感度、特异度分别为87.50%(70/80)、85.00%(68/80),有12例误诊、10例漏诊;二者联合时敏感度和特异度分别为97.50%(78/80)、97.50%(78/80),有2例误诊、有2例漏诊(见表 2)。
检测方法 诊断切点 敏感度/% 特异度/% AUC (95%CI) ITT < 1.0 mm 90.00 87.50 0.734(0.672~0.786) BS/BSOB >1.0 87.50 85.00 0.721(0.667~0.773) 二者联合 ITT < 1.0 mm或BS/BSOB>1.0 97.50 97.50 0.869(0.771~0.927)
2.1. 2组胎儿间脑及中脑特征、IT及后脑结构的超声特征
2.2. 2组胎儿ITT、BS、BSOB和BS/BSOB比较
2.3. 不同方法鉴别OSB的效能分析
-
OSB是指病变部位背侧皮肤缺损、椎管内成分部分或全部内容物经过脊柱缺损处向后膨出的一种严重的先天性畸形,具有极高的致残率及致死率,其主要的处理方法为尽早选择终止妊娠以减少对孕妇的身体伤害[5-6]。以往,胎儿OSB的筛查主要依据母体或羊水中甲胎蛋白和乙酰胆碱酯酶增高来间接诊断,其特异性差、敏感性低,而近年来随着超声技术的发展与成熟,通过在中孕晚期或晚孕期显示胎儿颅内“柠檬头、香蕉小脑、小脑延髓池消失”等超声特征,可有效诊断OSB的发生,但如何能更早期、更准确地诊断胎儿OSB是本研究和当前学者们重点关注和解决的问题[7-8]。
近年来,有研究[9]显示,在OSB胎儿其颅内后脑结构会发生改变时,会使第四脑室即IT显示模糊或不显示,此时应高度警惕开放性脊柱裂的可能性。而有研究[10-12]表明,OSB胎儿在孕11周以前就已经有一定程度的改变,但由于在早孕期第四脑室很小而超声检查不易显示,而至晚孕期由于后颅窝变小亦影响第四脑室的显示,因此中孕期是观察第四脑室最佳时期,且可在测量NT的同时进行IT的观察和测量评估,从而评估OSB的发生。也有研究[13-15]显示,正常胎儿BS和BSOB随孕周的增加而增大,但两者的比值BS/BSOB随孕周的增大而减小,但当发生OSB时,由于IT缩小或消失,BS厚度相对增大、BSOB则变小,故BS/BSOB比值将增大,提示其也可作为评估OSB发生的重要依据。
而在过往的研究中,不管使用哪种观测方法,都具有一定的局限性,且并未界定正常与OSB胎儿透明层及后脑结构参数的相应参照范围,对此,本研究通过回顾性分析OSB和正常胎儿的透明层及后脑结构的超声特征,发现健康组IT可清晰显示、间脑和中脑呈现“8”字形态;OSB组脑室受压、颅后窝颅内结构移位、IT显示部分受碍且有不同程度的减小或消失,间脑和中脑呈现“8”字形态有不同程度的变形和扭曲。OSB组ITT、BS、BSOB明显低于健康组,BS/BSOB明显高于健康组,提示中孕早期ITT减少或消失和BS、BSOB减少、BS/BSOB增大是OSB发生的重要后脑结构超声特征。这可能是由于在OSB发生过程中,胎儿脑脊液的减少造成颅内压力的降低从而引发颅后窝结构发生向后移位,导致BS受压增粗、IT及小脑延髓池变窄或消失,使BSOB缩小[16],故表现为BS厚度在增加同时其BSOB则明显降低,同时ITT减少、BS/BSOB增大。
而ROC分析显示,在鉴别OSB的敏感度、特异度方面,ITT以 < 1.0 mm为临界值时,分别为90.00%、87.50%,BS/BSOB以>1.0为临界值时,分别为87.50%、85.00%,二者无明显差异,提示检测ITT、BS/BSOB可考虑作为鉴别OSB发生的重要参考指标。而研究中通过将ITT、BS/BSOB联合鉴别OSB发生时,其敏感度、特异度分别为97.50%、97.50%,优于二者单用时,提示二者联合时具有更佳的鉴别效能。这可能是由于在二者单独检测时,部分胎儿中脑导水管细小,超声有时不易显示第四脑室,或由于脑脊液渗漏至羊膜腔内,中脑导水管及第四脑室难以显示[17],从而影响BS、BSOB的测量,而俯卧位虽可清晰显示IT但也易因颅骨遮挡颅内像脑干等其他结构不能清晰显示[18],从而影响ITT的测量;同时,在测量时,可能受母体肥胖、腹壁厚度、胎位、测量者和阅片者经验或主观评价等因素影响[19-20],会使胎儿的IT、BS、BSOB不一定都能清晰显示,从而影响ITT、BS/BSOB的准确性,从而导致误诊、漏诊的发生;而二者联合时,有助于避免二者单独时存在的不足及不良因素的影响,从而提高对OSB的鉴别效能。此外,在实际工作中观察这些结构均需要将图像尽量放大并使用高分辨率的仪器和探头,胎方位尽量选择仰卧位,胎儿面部朝向探头,并在不同平面仔细分辨依次观察间脑、中脑、第四脑室、后颅窝池、NT、丘脑、大脑脚及中脑导水管,但若组织器官和头颅横切面颅内结构等观察不清,可联合使用阴道超声检查,以使透明层及后脑结构得以全面清晰显示。








 DownLoad:
DownLoad: