-
骨质疏松症是老年人群常见慢性疾病,好发于绝经后女性,当病人骨量下降时,骨折风险明显上升。骨质疏松性椎体压缩骨折(osteoporotic vertebral compression fractures,OVCFs)是骨质疏松症最严重的并发症之一,骨折部位出现严重疼痛,具有较高的致残率及死亡率[1]。经皮椎体后凸成形术(percutaneous kyphoplasty,PKP)是治疗OVCFs最常用的微创术式之一,通过骨水泥填充椎体间隙以恢复椎体高度,增加椎体强度及稳定性。随着OVCFs PKP病人基数的增加,术后邻椎骨折的报道逐渐增多,有报道[2]称27.8%的OVCFs病人PKP术后新发椎体骨折,其中68%发生于临近上下椎体,邻椎骨折已成为OVCFs PKP治疗后重要防治方向。对于PKP术后邻椎骨折,有学者建议采用保守治疗,但随着PKP手术经验的积累、穿刺技术以及骨水泥质量的进步,其临床治疗效果也逐渐得到完善[3]。我院近年对21例OVCFs PKP术后邻椎骨折病人再次进行PKP术治疗,获得良好的临床疗效。现作报道。
HTML
-
选择2015年6月至2018年1月于我院治疗的21例OVCFs PKP术后邻椎新鲜骨折病人,男5例,女16例,年龄(69.43±5.02)岁,胸椎10例(T9 2例,T11 6例,T12 2例),腰椎11例(L1 2例,L2 5例L3 3例L4 1例)。纳入标准:(1)OVCFs PKP术史,影像学检查确诊再发临近椎体骨折;(2)临近单节段骨折,无神经、脊髓受压症状,椎体后壁保持完整;(3)原手术节段≤2;(4)病人自愿进行手术治疗,随访时间超过1年。排除标准:(1)肿瘤、结核等引起的骨折;(2)合并椎体失稳需融合治疗;(3)非临近节段骨折;(4)合并严重心肺功能障碍等手术不耐受者;(5)原手术节段再次骨折。
-
首先采用C臂X射线机正、侧位透视定位骨折椎体,采用1%盐酸利多卡因行局部麻醉。调整C臂X射线机,使射线投照平行于终板,两侧椎弓根对称,并与棘突距离相同,选择责任椎体棘突旁开3~5 cm,于椎弓根投影外右侧2点、左侧10点外侧2~3 mm处进针并穿透骨皮质,侧位透视见穿刺位置满意后继续进入,直至到达椎体后壁2~3 mm处,将内芯取出并置入导针、套管,精细钻钻达椎体前1/3处。相同方法进行另一侧穿刺,精细钻取出后进行C臂X射线机透视,并置入配套可扩张球囊,适当进行球囊加压(压力范围100~220 psi)直至透视下患椎椎体复位达到术前高度,或已达到球囊预期扩张压力,将骨水泥调整至最佳推注状态,即拉丝期,缓慢注入骨水泥,胸椎注入4~6 mL,腰椎注入6~8 mL,待骨水泥进入患椎后壁约1/4处时停止推注,并在骨水泥分布满意、固化后取出手术装置。注意骨水泥固化期间尽可能保持骨水泥注射器静止,以免引起骨水泥不必要的扩散。术后当天卧床,抗感染治疗2 d,术后第二天即可佩戴支具下床活动,术后给予常规抗骨质疏松治疗,并随访监测骨密度情况。
-
术后1个月、6个月、1年评价随访指标,疼痛视觉模拟(VAS)评分[4]:共10分,采用VAS卡尺,0刻度无任何疼痛,10刻度为无法忍受的疼痛;Oswestry功能障碍指数(ODI)[5]:包括行走、提物、上下楼梯等10项基本生活动作,ODI指数=得分/总分×100%;伤椎前缘高度比=伤椎前缘高度/临近上下节段椎体前缘均值×100%;侧位X线片计算Cobb角;记录术后并发症情况。
-
采用方差分析和q检验。
1.1. 一般资料
1.2. 方法
1.3. 观察指标
1.4. 统计学方法
-
所有病人均成功完成手术,手术用时(49.45±6.43)min,出血量(23.23±4.87)mL,骨水泥注入量(4.91±1.21)mL。
-
术后1个月、6个月、1年VAS评分和Cobb角明显低于术前,ODI指数和椎体前缘高度比明显高于术前(P < 0.01);术后6个月、1年的VAS评分低于术后1个月(P < 0.05)、ODI指数高于术后1个月(P < 0.01);术后1年椎体前缘高度比低于术后1个月和6个月(P < 0.05)(见表 1)。
指标 术前 术后1个月 术后6个月 术后1年 F P MS组内 VAS评分/分 7.21±1.21 2.65±0.22** 2.12±0.20**# 2.14±0.16**# 323.58 < 0.01 0.395 ODI指数/% 46.22±6.85 78.62±7.34** 87.11±7.23**## 88.09±6.65**## 164.54 < 0.01 49.323 Cobb角/(°) 18.22±3.15 7.62±0.94** 7.81±0.73** 8.17±6.25** 44.75 < 0.01 12.600 椎体前缘高度比/% 63.23±6.34 90.23±3.24** 89.82±3.71** 86.03±6.88**#▲ 124.48 < 0.01 27.948 q检验:与术前比较**P < 0.01;与术后1个月比较#P < 0.05,##P < 0.01;与术后6个月比较▲P < 0.05 -
术后3例病人出现慢性腰痛,经物理治疗缓解;无切口感染、骨水泥渗漏、椎体再骨折等并发症出现。
-
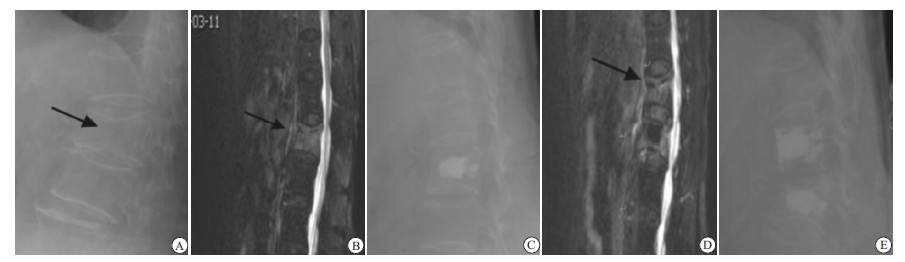
典型病例见图 1。
2.1. 手术完成情况
2.2. 手术前后影像及功能症状指标比较
2.3. 术后并发症情况
2.4. 典型病例
-
有报道[6]称,初发OVCFs病人不经外科干预邻近椎体骨折率为19.2%,而经PKP、经皮椎体成形术治疗后这一比例上升至28.7%。研究[7]显示,年龄较大、未进行系统抗骨质疏松治疗、术后骨水泥渗漏、骨密度过低是单节段OVCF病人PKP术后临近椎体骨折的独立危险因素。其中年龄较大、骨密度过低、未进行规范治疗者临近椎体骨折主要因为骨质流失,骨脆性增加;骨水泥渗漏后患椎椎间盘应力降低,而邻近椎体所受应力加强,发生骨折分析增大。
随着PKP治疗的OVCFs病人逐年增多,术后邻椎骨折病例基数也逐渐增大,在邻椎骨折的治疗方式、时机上仍存在一定的争议。卧床制动、佩戴胸腰支具、配合药物抗骨质疏松治疗是邻椎骨折最简单的治疗方案,但绝对卧床制动时间过长可能引起骨质流失加剧以及压疮、心肺相关并发症等[8-9]。随着PKP手术经验的积累、穿刺技术以及骨水泥质量的进步,PKP运用更加广泛。但有报道[10]认为,PKP注入骨水泥后,胸腰椎受力方向、顺应性、生物力学均有所改变,而这种变化随着手术节段的增多而增大,尤其是造成胸腰椎受力轴线前移,前缘受力增加,易造成手术节段及临近节段的再次骨折。因此,考虑到手术的安全性以及排除干扰项,本研究纳入病例时严格控制了适应证,仅纳入原骨折节段≤2及再次骨折为单节段者。
本研究21例病人均成功完成手术,术后各随访时间VAS评分、ODI指数、Cobb角均明显低于术前,椎体前缘高度比高于术前,表明PKP在OVCFs PKP术后邻椎骨折治疗中的有效性。术后1年伤椎Cobb角、椎体前缘高度比低于术后1个月,但矫正丢失属于正常范围。在手术治疗中常规穿刺后可扩张球囊的使用能有效保护压缩病灶周围的椎体骨质,尤其对于骨质疏松者,能降低骨水泥灌注后向椎体后壁渗漏的风险[11]。同时,可扩张球囊的压力具有可调整性,能够满足病人的个性化扩张,从而提高椎体成形术对注入骨水泥量的把握,降低了骨水泥过量或不足导致的骨水泥渗漏与锥体高度无法恢复的风险[12]。本研究PKP术后无切口感染、骨水泥渗漏、椎体再骨折等病发症出现。PKP术治疗OVCFs PKP术后邻椎骨折的手术方法与初发OVCFs并无明显差别,但需要针对邻椎骨折的危险因素注意术中操作,例如穿刺针到达椎体后壁2~3 mm处为宜,把握术中骨水泥注入量,同时术后检测骨密度并给予针对性治疗[13-14]。综上所述,OVCFs PKP术后邻椎骨折再次经PKP治疗能有效降低疼痛症状,恢复椎体高度,手术安全有效,但需要注意手术技巧,术后规范抗骨质疏松治疗。






 DownLoad:
DownLoad: