-
食管癌是消化系统常见的恶性肿瘤之一,据2018年公布的统计数据,我国食管癌发病率居恶性肿瘤中的第6位[1]。临床上具有早期症状不明显,误诊率和漏诊率高的特点。食管癌最易出现淋巴结转移,一旦发生转移,治疗难道增大,严重影响病人的生活质量及生存时间[2]。因此,术前明确病人是否存在淋巴结转移以及转移数目和范围,直接影响临床治疗方案的选择和预后评估。当前食管癌常用的影像学检查主要是X线钡餐造影、传统CT平扫及增强等。X线钡餐造影可较直观地显示病变部位、大小、形态,但无法显示腔外侵犯和淋巴结转移情况。传统CT扫描是诊断食管癌淋巴结转移最常用的方法,通常依据淋巴结的大小及形态学来判断是否存在淋巴结转移,但敏感性不高,存在较高的漏诊率和误诊率[3];且传统CT的X线属于混合能量射线,图像的判读容易受射线束硬化伪影的影响[4]。近来随着CT技术的不断发展,能谱CT成像因其多参数成像的优势,在食管癌术前诊断中的应用逐渐增多[5-6]。本研究旨在探究CT能谱成像在定性判断不同分化食管癌淋巴结转移中的应用价值。
HTML
-
选取2019年3-12月在蚌埠医学院第一附属医院进行手术的48例食管癌病人作为研究对象,其中男31例,女17例,年龄48~76岁。纳入标准:(1)经胃镜病理检查诊断为食管鳞癌;(2)行CT扫描前均未进行任何治疗,且扫描结束后1周内行外科手术治疗;(3)无其他恶性肿瘤病史;(3)无碘过敏史及其他相关检查禁忌证。排除标准:(1)伴肝、肾等严重功能不全者;(2)影像学或病理资料不全者;(3)伴甲状腺功能亢进者;(4)图像质量差不满足诊断要求者。
-
能谱CT检查前3 d禁行上消化道造影检查,检查当天禁食6~8 h,扫描前10~15 min内肌肉注射消旋山莨菪碱20 mg,检查前饮水800~1 000 mL以充盈上消化道,检查取仰卧位后,用吸管饮水200~300 mL以充盈食管。采用GE公司Revolution 256排CT的GSI模式行平扫+动静脉期增强双期扫描,管电压以0.5 ms在80 keV、140 keV之间瞬时切换,管电流550 mA,扫描范围自锁骨上区至肝脏下缘水平,对比剂选用碘海醇(欧乃派克,350 mg/mL)80~100 mL,利用高压注射器经右侧前臂肘静脉注入对比剂,速率为3.0 mL/s,于对比剂注入后30 s行动脉期增强扫描,60 s行静脉期扫描,层厚5 mm、层间距5 mm,后处理自动重建成层厚0.625 mm、层间距0.625 mm的能谱序列图像。
-
扫描完成后相关数据自动传至GE AW 4.7工作站,选中相应能谱序列数据,用GSI Protocols general软件进行分析和观测,纵隔淋巴结分组参照美国癌症联合会联合国际抗癌联盟标准[7],标记胸内各组淋巴结,测量、记录大小,同时测量其动脉期70 keV单能量下的CT值(CT70 keV)和碘基图上淋巴结动、静脉期碘浓度,并与同层面主动脉碘浓度相比,计算淋巴结动、静脉期标准化碘浓度(normalized iodine concentration,NIC)。结合食管癌病灶及淋巴结能谱曲线,诊断淋巴结性质,并与手术后病理结果进行比较。
-
采用t检验、配对χ2检验和ROC曲线分析。
1.1. 一般资料
1.2. 检查方法
1.3. 图像分析
1.4. 统计学方法
-
48例食管癌病人中,病变位于上段5例,中上段4例,中段17例,中下段8例,下段14例。高分化鳞癌11例,中分化鳞癌15例,低分化鳞癌22例。
-
48例食管癌病人中,食管癌手术及病理证实伴淋巴结转移32例,无淋巴结转移16例。在食管癌CT能谱图像上相应标记淋巴结总共111枚,手术后经病理结果证实转移淋巴结共79枚,其中高、中、低分化鳞癌转移淋巴结分别是14枚、27枚和38枚;非转移性淋巴结32枚,能谱CT成像诊断淋巴结转移与手术后病理结果差异无统计学意义(P>0.05)(见表 1)。
分组 病理转移 病理非转移 合计 χ2 P 能谱CT转移 68 4 72 3.27 >0.05 能谱CT非转移 11 28 39 合计 79 32 111 -
高中分化食管鳞癌转移性淋巴结短径、动脉期CT70 keV、动静脉期NIC均高于非转移性淋巴结(P < 0.05~P < 0.01)(见表 2)。低分化食管鳞癌转移性淋巴结短径、动脉期CT70 keV、动静脉期NIC均高于非转移性淋巴结(P < 0.05~P < 0.01)(见表 3)。
分组 n 短径/mm 动脉期CT70 keV/Hu 动脉期NIC 静脉期NIC 转移淋巴结 41 9.37±2.95 69.52±18.23 0.24±0.07 0.63±0.10 非转移淋巴结 32 6.52±3.02 51.79±14.48 0.15±0.05 0.44±0.15 t — 2.12 4.50 6.15 6.48 P — < 0.05 < 0.01 < 0.01 < 0.01 分组 n 短径/mm 动脉期CT70 keV/Hu 动脉期NIC 静脉期NIC 转移淋巴结 38 9.48±3.24 76.64±23.21 0.31±0.09 0.52±0.12 非转移淋巴结 32 6.52±3.02 51.79±14.48 0.15±0.05 0.44±0.15 t — 3.93 5.25 8.95 2.48 P — < 0.01 < 0.01 < 0.01 < 0.05 -
动脉期CT70 keV、动脉期NIC和能谱曲线斜率诊断食管癌转移性淋巴结的AUC值(95%CI)分别为0.75(0.69~0.82)、0.82(0.78~0.91)、0.80(0.73~0.86),当动脉期CT70 keV的阈值为65.22 HU时,敏感度和特异度分别为73.8%、82.2%;当动脉期NIC阈值为0.19时,敏感度和特异度分别为82.9%、85.4%;当动脉期能谱曲线斜率阈值为1.32时,敏感度和特异度为78.6%、81.1%。动脉期CT70 keV、动脉期NIC及能谱曲线斜率联合诊断食管癌转移淋巴结的敏感度和特异度分别为86.1%和87.5%。
-
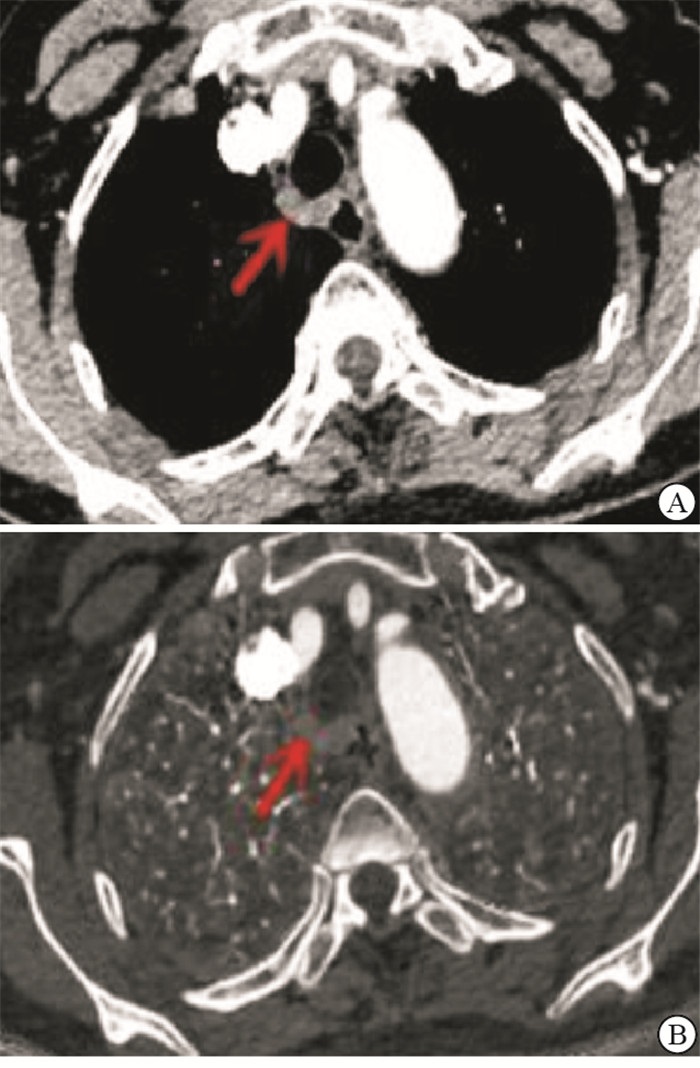
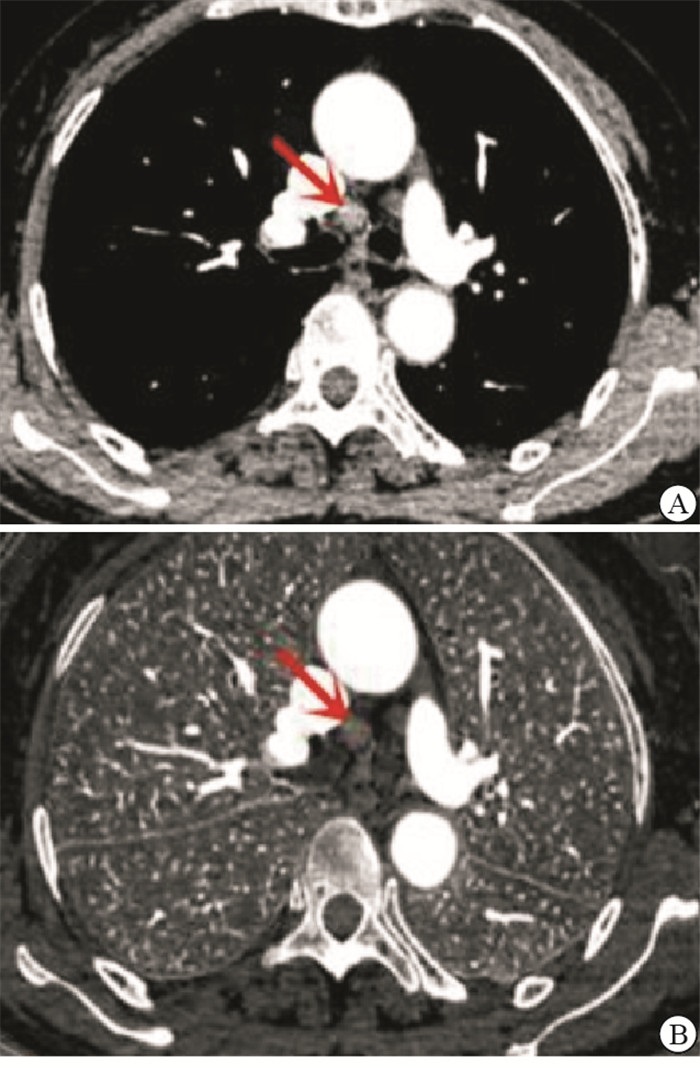
病例1,男,64岁,食管中下段低分化鳞癌,主肺动脉窗淋巴结转移(见图 1)。病例2,女,55岁,食管下段高分化鳞癌,气管隆突下淋巴结转移(见图 2)。病例3,男,67岁,食管中上段高分化鳞癌,气管旁非转移淋巴结(见图 3)。
2.1. 48例食管癌病人的基本情况
2.2. 能谱CT诊断食管癌淋巴结转移的总体情况
2.3. 高中分化、低分化食管鳞癌不同性质淋巴结短径、动脉期CT70 keV、动脉期及静脉期NIC比较
2.4. ROC曲线分析
2.5. 典型病例
-
全世界每年死于食管癌的病人超过22万[8],我国更是食管癌的高发国家,严重威胁着人类的健康和生活质量。在食管癌的治疗中,准确判断淋巴结的转移数量和转移范围是食管癌N分期的关键,也是临床医师一直关注的重点,因其与病人治疗方案的选择及预后评价息息相关。临床工作中通常用的常规CT检查来诊断食管癌淋巴结转移情况,常将除气管食管旁沟淋巴结短径>5 mm外,其他各区域淋巴结短径>10 mm时,定性为转移性淋巴结,但其对食管癌术前淋巴结转移诊断灵敏度仅为62.86%[9],研究中发现仍有部分病人出现淋巴结术前分期不准的情况,其误诊或漏诊的原因主要是一方面食管癌中晚期病人常会出现良性反应性淋巴结肿大;另一方面一些短径较小的淋巴结也可能是转移性淋巴结。能谱CT成像利用不同X线能量下物质吸收不同的原理,提供相比传统CT更多的影像学图像信息,经过运算可以获得101个单能量图像(40~140 keV)、能谱曲线、基物质图及有效原子序数等[10],从而可以对食管癌进行多参数分析。依据食管癌病灶与其转移性淋巴结之间的同源性,本研究通过能谱CT成像对不同分化程度食管鳞癌转移性淋巴结与非转移性淋巴结的动脉期CT70 keV、动脉期及静脉期NIC多参数的分析,发现能谱CT诊断转移性淋巴结的优越性,其敏感度明显高于传统CT,打破了传统CT仅依赖淋巴结大小及形态的诊断模式。
转移性淋巴结与非转移性淋巴结有不同的病理表现,食管鳞癌转移性淋巴结因肿瘤细胞浸润,正常组织细胞被取代,淋巴结原有组织结构及血供发生了改变;非转移性淋巴结包括正常淋巴结或由感染引起的炎性细胞增生或反应性肿大的淋巴结。这些不同的病理表现造成了转移性淋巴结与非转移性淋巴结不同的X衰减系数的变化。然而传统CT难以检测出这些变化。能谱CT成像作为一种新兴的多参数成像的影像检查方法,其特有的单能量图像可以反映淋巴结不同病理变化所致的X线衰减系数的变化。单能量图像最大的优势是根据成像条件来改善CT值的漂移获得最佳的图像,有研究[11]指出70 keV时的单能量图可以提高组织之间的对比性,获得较好的信噪比,显示转移性淋巴结最清晰。动脉期CT70 keV、动静脉期NIC可以间接地反映不同性质的淋巴结血供的变化[12]。本研究高中分化食管鳞癌、低分化食管鳞癌的转移性淋巴结与非转移性淋巴结的动脉期CT70 keV、动脉期及静脉期NIC差异均有统计学意义,说明转移性淋巴结与非转移性淋巴结之间强化程度存在差异,这与丁聪等[13]的研究结果一致。
不同分化食管鳞癌转移性淋巴结能谱参数存在差异。不同分化食管鳞癌转移性淋巴结组织中血供情况和组织机构的不同可能是造成能谱CT参数差异的重要原因;恶性程度越高及组织分化越差的肿瘤,其转移性淋巴结组织中微血管密度越高,碘浓度就越高[14-15]。食管癌不同病理分级会有不一样的单能量CT值,癌组织分化程度越好对应的单能量CT值越低,癌组织分化程度越差对应的单能量CT值则相对较高[16]。能谱CT碘基图能够定量分析组织中碘的分布及浓度,间接反映组织的血流动力学情况[17]。本组研究用淋巴结动脉期CT70 keV以及动脉期和静脉期NIC参数对不同分化食管鳞癌转移性淋巴结进行观测,并与术后病理结果进行比对,结果证实了不同分化食管鳞癌转移性淋巴结能谱参数存在差异。研究中也发现小部分转移性淋巴结的动脉期CT70 keV及动静脉期NIC均较低,其原因可能与部分低分化食管鳞癌的转移性淋巴结出现明显坏死,导致血供差,摄碘能力低有关;另外病人的自身循环因素及扫描条件的差异也可能影响淋巴结CT70 keV和碘浓度。
综上所述,CT能谱成像在定性评估不同分化食管癌转移性淋巴结中具有较高价值,可以为临床诊断食管癌淋巴结转移提供更加有效的方法,从而为病人制定治疗方案提供有利治疗依据,值得在临床中推广。









 DownLoad:
DownLoad: