-
目前国内外研究发现,子痫前期是一种多系统高血压疾病,且重度子痫前期是引起全球围生期疾病和死亡的重要因素之一[1-3]。虽然目前主要机制和发生率不清楚,但是确实在子痫前期的部分病人中颅内压(intracranial pressure,ICP)升高时有发生[4]。目前评估ICP仍以有创ICP监测为主,但有创监测有多种禁忌证,且有出血、感染等并发症,临床应用受限,并不适合于孕产妇[5]。近年来国内外大量研究[6-8]表明,超声测量视神经鞘直径(ONSD)用于评估ICP具有无创、准确、可重复性高等特点。国内外鲜有重度子痫前期病人ONSD值的超声研究,本文研究孕妇的ONSD与重度子痫前期ICP增高的相关性,研究其ICP增高时ONSD的最佳阈值,为诊断和治疗重度子痫前期ICP增高提供一定依据。
HTML
-
2018年8月至2020年1月在蚌埠医学院第一附属医院诊断为疑似子痫前期的44例单胎孕妇作为观察组,同时收集30例排除合并症的单胎孕妇为对照组。排除标准:明确表示拒绝、眼部外伤、眼部手术史或存在其他眼病史病人[9]。纳入标准:(1)病人出现头疼、视觉障碍、弥漫性脑水肿、意识模糊、视乳头水肿等ICP增高的疑似症状。(2)符合子痫前期的诊断标准,即妊娠≥20周后首次出现收缩压≥140 mmHg或舒张压≥90 mmHg,均进行2次测量,每次均符合要求,并且测量时间间隔至少6 h,蛋白尿≥0.3 g/24 h[10]。另外收集孕妇的孕周、孕产次数、年龄、体质量等基线信息。
-
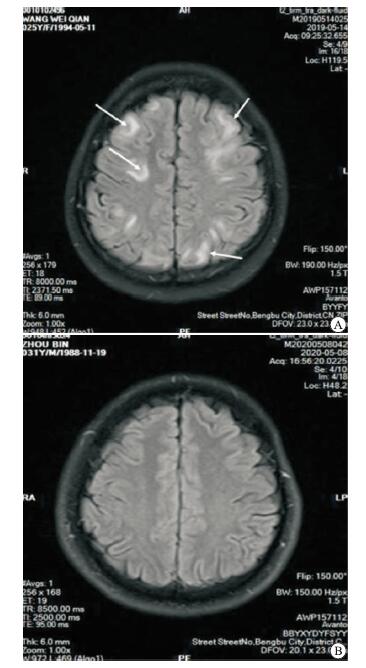
对照组的孕妇仅进行ONSD的测量,而观察组的孕妇需进行MRI和ONSD的检测和测量。采用SonoSite M-Turbo超声诊断仪5~10 MHz超声探头检查:经眼眶部位测量所有孕妇同一侧眼球后3 mm处的ONSD值,均需测量3次并算取平均值作为该孕妇的ONSD测量值(见图 1);对孕妇ICP增高的评定根据此孕妇的MRI检查结果判断(经同一位有丰富临床经验的影像学医生的判断):以MRI结果出现颅脑内出现异常,出现脑室、脑池、脑沟等改变,并出现脑水肿症状即为ICP增高[11]。此外,关于本研究的所有孕妇的基础临床资料对作为观察者的影像学医生设盲,观察组仅根据MRI实际检测结果分为ICP正常组和ICP增高组(见图 2)。
-
采用单因素方差分析、q检验,使用受试者工作特征曲线(ROC)并计算特异度和灵敏度。
1.1. 一般资料
1.2. 方法
1.3. 统计学方法
-
44例疑似子痫前期孕妇中可疑ICP增高的孕妇是19例(43.18%);最终依据MRI结果判断ICP增高的孕妇为14例(34.09%),结果显示,3组间孕妇的年龄、孕产次比较,差异均无统计学意义(P>0.05)。3组间收缩压、舒张压、孕周和ONSD值比较,差异均有统计学意义(P < 0.01)。其中收缩压和舒张压ICP增高组均显著高于ICP正常组和对照组,ICP增高组显著高于ICP正常组(P < 0.01);孕周对照组显著高于ICP正常组和ICP增高组;ONSD值ICP增高组和正常组显著高于对照组,ICP增高组显著高于ICP正常组(P < 0.01)(见表 1)。
分组 n 年龄/岁 收缩压/mmHg 舒张压/mmHg 孕产次 孕周 ONSD/mm 对照组 30 31.1±5.0 117.0±10.0 74.0±5.0 2±1 40.5±2.9 3.90±0.10 ICP增高组 14 30.0±7.0 157.0±23.0** 105.0±20.0** 2±1 36.1±4.2** 4.70±0.30** ICP正常组 30 29.3±4.5 121.0±15.0## 76.0±13.0## 3±1 37.5±3.9** 4.10±0.10**## F — 0.87 34.89 30.47 1.897 8.759 102.78 P — >0.05 < 0.01 < 0.01 >0.05 < 0.01 < 0.01 MS组内 — 27.454 229.606 152.479 2.000 13.100 0.000 与对照组比较**P < 0.01;与ICP增高组比较##P < 0.01 -
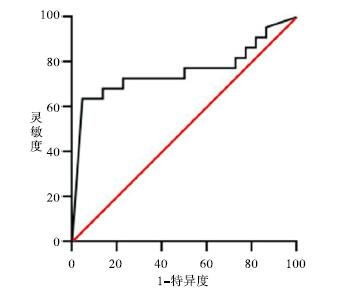
超声ONSD筛查44例疑似子痫前期孕妇ICP增高的ROC曲线,其ROC曲线下面积(AUC)为0.759(P < 0.01),最大约登指数指数为0.497,对应的当ONSD值是4.0 mm为重度子痫前期病人的ICP增高最佳临阈值,此时的灵敏度和特异度分别为62.2%、87.5%(见图 3)。
2.1. 孕妇一般资料及ONSD值
2.2. 利用ONSD值对ICP增高的重度子癫痫孕妇的诊断
-
子痫前期是全球孕产妇死亡的第二大原因,主要是由于急性脑并发症的发生[12-13]。有关其发病机制尚未明确,发病率全球各地差异也较大,有报道在全部妊娠中的发病率3.2%~12%[14-16],根据最新的报道显示,我国的发病率为4.2%[17]。ICP升高是子痫前期孕妇临床常见的综合征,一般ICP的增高由颅脑损伤、脑肿瘤、脑出血、脑积水和颅内炎症和感染等引发。ICP增高有时会引发脑疝危象,可使病人因呼吸循环衰竭而死亡。国外报道[18-19]指出,有71%~100%重度子痫前期的病人存在MRI表现脑水肿和ICP增高的情况。如何及时采用便捷的方式诊断子痫前期ICP增高,便于临床医生进行有效的治疗是目前亟需解决的首要问题。尽管目前有创性的ICP监测是临床首选,但是该检查有多种禁忌证,侵入性检测可能会引发感染、出血等风险[5],所以有创的ICP监测对于需求保守治疗的子痫前期孕妇并不适用。临床迫切需求准确、简单、无创的技术用于评估和监测孕妇的ICP增加情况。
目前临床常用的无创ICP增高的辅助检测方法日益增多,包括经颅多普勒(TCD)、CT、MRI等并且各有优劣。目前TCD在无创ICP监测方面临床的认可度和普及度高,但是TCD对医生的专业性要求较高,临床普遍开展收到限制。头颅CT及MRI影像学检查近年来由于其灵敏度高、可重复等特点,通过评估脑水肿、脑中线结构移位等可间接诊断ICP增高[20-21]。虽然低剂量的辐射被证实是安全的,但是孕妇是普遍是拒绝CT检查的,另外MRI由于耗时长、检查花费高等问题,造成两者未能在临床上普及和开展。通过ONSD值变化规律可反应ICP增高的情况,近年来越来越多的证据支持ONSD检查可以为临床判定ICP增高提供参考依据[22-24]。由于经眼眶超声测量ONSD具有快速、廉价、无创、可重复性高等特点使其在临床普及更具有优势。
视神经作为中枢神经系统的一部分,被硬膜鞘和含有脑脊液的蛛网膜下腔所包围。在眼球后方3 mm处,视神经仅被脂肪包围,而硬膜鞘在其脂肪包裹下是可膨胀的,特别是在脑脊液压力升高的情况下。所以由于这种特殊的构造,随着ICP的增高势必导致ONSD值增加[25]。本研究发现,ONSD值的ICP增高组比ICP正常组和对照组明显升高(P < 0.01),但是ICP正常组与对照组差异无统计学意义(P>0.05),与利青等[26]测量了70例妊娠高血压疾病孕妇的结果一致。本研究的ICP增高组的ONSD值为(4.70±0.30)mm,较之前研究数值偏小,如2017年利青等[26]研究的结果为(5.80±0.40)mm,2020年渠晓旭等[22]研究结果为(5.30±0.69)mm。造成这种情况的原因一方面可能由于人群差异导致ICP增高情况不同,另一方面本研究中样本量较小在一定程度上可能会造成偏倚。本研究发现子痫前期孕妇ICP增高的ROC曲线为0.759,一定程度可以判断ONSD在诊断ICP增高具有临床意义。此外,研究发现当ONSD值是4.0 mm为子痫前期病人ICP增高的最佳阈值,与国内外研究中心对ONSD诊断ICP增高的临界值相符(4.00~6.00 mm),目前业内一直认为临界阈值取5.0 mm[27-29]。但ICP增高如果得不到及时处理,特别是重度子痫前期病人会出现严重的后果甚至导致死亡,所以关于ONSD诊断ICP的临界值研究支持 < 5.0 mm。目前国内外一直认为超声检查ONSD在临床诊断ICP增高是一种潜力的无创工具,但是对于ONSD用于诊断子痫前期孕产妇ICP增高情况的研究鲜有报道,本研究对诊断和治疗重度子痫前期ICP增高提供依据。
本研究可能存在以下不足:(1)研究为蚌埠医学院第一附属医院单中心研究,样本量少,结果可能会有一定的偏倚;(2)本研究的研究对象为孕妇,所以未使用侵入性ICP监测,使用MRI间接判断ICP增高势必存在假阴性和假阳性的可能;(3)运用经眼眶超声测量ONSD是需要具有丰富经验的该专业的临床医生完成,具有较高的专业诉求,可能会在后期的临床普及上受到一定的限制。
综上所述,本研究结果显示利用ONSD值对ICP增高的重度子痫孕妇的诊断具有可靠的灵敏度和特异度。超声监测ONSD与重度子痫前期ICP增高有良好的相关性,为以后此类病人的实时监测,降低ICP升高带来的风险,提供帮助。医生可以根据ONSD及数值的变化及时掌握子痫前期孕妇ICP增高的情况并及时做出应对策略,适合在医院妇产科推广和应用。










 DownLoad:
DownLoad: