-
急性播散性脑脊髓炎(acute disseminated encephalomyelitis, ADEM)是一种中枢神经系统自身免疫性脱髓鞘性疾病,儿童为主要受累者。因本病临床症状非特异且缺乏有效的生化指标,故目前儿童ADEM的诊断缺乏金标准,预后判断困难;既往儿童ADEM的文献多是小样本量和短期随访,本文报道较大样本量和较长随访时间的研究结果,期望进一步阐释儿童ADEM的临床特点,并对随访到的患儿进行分组,对可能影响本病预后的多种因素进行分析。现作报道。
HTML
-
2012年1月至2018年7月我科收住确诊的ADEM患儿,共77例,其中男44例(57.1%),女33例(42.9%),男女比例4∶3;发病年龄4月14天至14岁。
-
参照国际儿童多发性硬化研究组(IPMSSG)儿童ADEM诊断标准[1],符合以下所有条件: (1)第1次多灶性临床中枢神经系统事件,推定原因为炎症性脱髓鞘。(2)不能用发热解释的脑病症状。(3)发病3个月或以上不出现新的临床或MRI病灶。(4)急性期(3月内)脑或脊髓MRI异常。(5)典型的脑MRI表现为:①弥散的、边界欠清晰的、较大的(>1~2 cm)病灶,主要累及脑白质;②脑白质区T1低信号病变少见;③深部灰质核团可存在病灶。(6)排除病原体直接感染疾病、遗传代谢疾病、结缔组织病及肿瘤等所致脑脊髓病。
-
回顾性分析患儿住院期间的临床资料,门诊及电话随访患儿情况。分组设计病例对照研究,分组依据[2]:痊愈组和不完全痊愈组,痊愈组随访时无症状,无治疗;不完全痊愈组遗留临床症状或病情反复(仍达不到其他免疫性疾病诊断指标),遗留症状包括:肢体不灵活或伴语言功能差,尿床,头痛,抽搐,包括死亡。对2组的性别、发病年龄、病前诱因、主要临床症状、脑脊液(CSF)白细胞及蛋白水平,四肢肌电图、头颅MRI进行统计分析。
-
采用χ2检验和Fisher′s精确概率法。
1.1. 一般资料
1.2. 入组标准
1.3. 研究方法
1.4. 统计学方法
-
56例感染后发病,其中上呼吸道感染52例,肺炎3例(包括支原体肺炎1例),腹泻1例;3例有疫苗接种史无感染;4例同时有疫苗接种史及上呼吸道感染诱因;14例(18.2%)无明确诱因。
-
诱因:病前感染77.9%,疫苗接种9.1%;临床症状:发热39.0%,肢体活动障碍37.7%,惊厥33.8%,意识障碍24.7%,头痛头晕19.5%,二便障碍10.4%,口眼歪斜7.8%,视物不清5.2%,共济失调5.2%,精神行为异常3.9%;神经系统体征:肌肉减退37.7%,病理征23.4%,脑膜刺激征9.1%。
-
69例患儿入院后接受腰穿CSF检查,其中34例(49.3%)有核细胞数增高,16例(23.2 %)蛋白增高。15例CSF与血清同步送检寡克隆区带(OB)、碱性髓鞘蛋白(MBP),仅1例血清和CSF均OB阳性,该例患儿CSF常规、生化正常,其他14例血清和CSF的OB、MBP均为阴性,其中1例存在CSF的IgG鞘内合成。5例检测CSF及血清的髓鞘少突胶质细胞糖蛋白(MOG)抗体,CSF均阴性,2例血清阳性。16例检测血清支原体IgM抗体,其中10例阳性。6例检测CSF支原体IgM抗体,均为阴性。
-
55例入院后接受脑电图检查,36例(65.5%)异常,表现为轻重不等的背景慢波,偶见局灶性异常放电。29例接受肌电图检查,异常11例(37.9%),表现为双侧对称性CMAP波幅低,或运动感觉神经传导速度减慢,或F波波幅低或出波率低。15例患儿接受视觉诱发电位检查,7例(46.7%)有异常,表现为P100潜伏期延长或伴波形分化差。
-
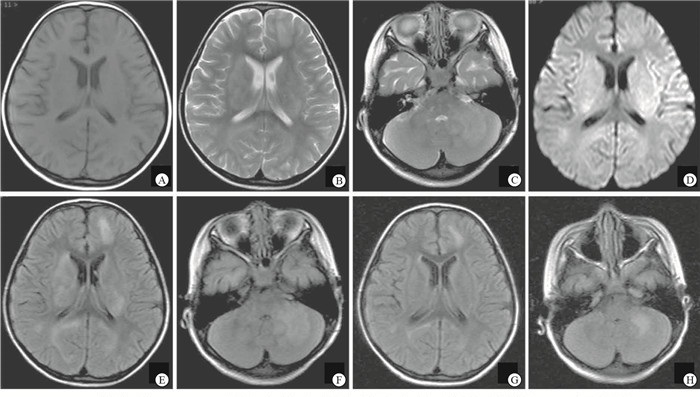
76例入院后接受头颅MRI检查,66例(86.8%)异常(见图 1),56例接受脊髓MRI检查,27例(48.2%)异常。10例头颅MRI正常患儿,依据脊髓MRI异常信号诊断。
-
75例患儿在对症、支持治疗基础上,采用免疫治疗方案,10例患儿仅用糖皮质激素治疗,3例患儿仅用免疫球蛋白治疗,62例患儿同时应用免疫球蛋白联合糖皮质激素治疗。应用糖皮质激素治疗患儿后续泼尼松1~2 mg·kg-1·d-1口服,逐渐减量,总疗程3~5月。
-
77例患儿,4例表现为ADEM多相型:第1例病史3年,停药2年半再发;第2例病史半年,停药10 d再发;第3例病史10个月,减药量过程中反复;第4例病史2个月,治疗好转后复查头颅MRI见新病灶。4例中有3例检测了CSF的OB、MBP和IgG鞘内合成,均正常;2例检测了CSF和血清MOG,1例为血清阳性、CSF阴性,另1例血清及CSF均为阴性。
-
随访到患儿41例,随访时间为病后6个月至6年6个月,根据随访结果分为2组:痊愈组和不完全痊愈组,其中痊愈组31例,患儿临床症状消失,无治疗;不完全痊愈组包括运动能力下降2例,病后尿床1例,抽搐伴语言运动能力下降1例,头痛1例,无症状、口服泼尼松治疗中1例,病情反复需继续治疗1例,严重双下肢无力、萎缩伴二便障碍1例,死亡2例(1例治疗稳定数月可上学,突发抽搐、呼吸衰竭死亡,另1例病情重,治疗中死亡)。
-
2组患儿性别、发病年龄、病前诱因、临床主要症状、CSF白细胞及蛋白水平、四肢肌电图、头颅MRI差异均无统计学意义(P>0.05) (见表 1)。
变量 痊愈组(n=31) 不完全痊愈组(n=10) χ2 P 性别 女 15(48.4) 6(60.0) 0.08 >0.05 男 16(51.6) 4(40.0) 年龄/岁 < 2 5(16.1) 3(30.0) — >0.05* 2~5 10(32.3) 2(20.0) >5 16(51.6) 5(50.0) 肢体活动障碍 11(35.5) 3(30.0) 0.00 >0.05 症状 惊厥 7(22.6) 4(40.0) 0.45 >0.05 意识障碍 7(22.6) 4(40.0) 0.45 >0.05 头痛头晕 7(22.6) 1(10.0) 0.17 >0.05 发热 10(32.3) 2(20.0) 0.12 >0.05 诱因 疫苗接种 1(3.2) 1(10.0) — >0.05* 前驱感染 19(61.3) 10(100.0) 3.76 >0.05 CSF白细胞 异常 15(53.6) 5(55.6) 0.00 >0.05 正常 13(46.4) 4(44.4) CSF蛋白 异常 8(28.6) 4(44.4) 1.15 >0.05 正常 20(71.4) 5(55.6) 四肢肌电图 异常 4(30.8) 3(75) 0.98 >0.05 正常 9(69.2) 1(25) 头颅MRI 有基底核或脑干病灶 11(36.7) 4(40) 0.00 >0.05 无基底核或脑干病灶 19(63.3) 6(60) *示Fisher′s确切概率法P值
2.1. 发病诱因
2.2. 临床症状及神经系统体征
2.3. 辅助检查
2.3.1. 血清及CSF检测
2.3.2. 神经电生理检查
2.3.3. 神经影像学检查
2.4. 治疗
2.5. 多相型病例
2.6. 随访结果
2.7. 2组随访患儿变量比较
-
目前认为ADEM是由于某些病原体的氨基酸序列和人髓鞘蛋白的氨基酸序列相似,病原体感染后发生抗原抗体反应导致的免疫损伤性疾病,患儿常有病前感染或疫苗接种史。ADEM临床症状复杂多样、缺乏特异性,CSF及血液化验无明显特征性,影像学表现常为诊断的重要依据[3]。需与多发性硬化、视神经脊髓炎、急性横贯性脊髓炎、神经系统其他免疫或代谢性疾病等鉴别。治疗主要是糖皮质激素、免疫球蛋白和对症治疗。
本组患儿在发病诱因、临床症状构成、辅助检查情况、预后等与文献[4]报道基本一致。病前感染率77.9%,疫苗接种率9.1%。临床症状按发生频率排序:发热,肢体活动障碍,惊厥,意识障碍,头痛头晕,二便障碍,口眼歪斜,视物不清,共济失调,精神行为异常等,其中非特异症状以发热多见,病程中有发热,但临床症状体征不能用发热解释。ADEM患儿的CSF和血清中可检测到异常免疫球蛋白,这些免疫指标对鉴别诊断有一定意义[5]。本组少部分病例检测了CSF和血清OB、MBP、MOG及支原体IgM抗体这些免疫指标,阳性率低,符合儿童ADEM病因单纯、预后良好的特点。ADEM病灶广泛累及中枢,但近年不少同时存在周围神经损害的报道[6-7],本组肌电图检查异常率37.9%,证实周围神经损害的存在。本组病例头颅MRI阳性率86.8%,脊髓MRI阳性率48.2%,支持儿童ADEM的诊断以影像依据为重[8]。
ADEM多为单相病程,多相型ADEM指发生2次符合ADEM诊断标准的临床事件,2次间隔至少3个月,第2次事件可以是前一次的原病灶复发,也可以出现新的临床或MRI病灶[1]。KOELMA等[5]回顾性观察了228例ADEM病人,其中112例为儿童,认为儿童ADEM复发多数应诊断为多相型ADEM,成人更多可诊断为多发性硬化。PAPETTI等[9]研究发现CSF中存在OB是儿童ADEM向多发性硬化转化的预测指标。本组观察ADEM患儿77例,多相型4例,其中3例接受免疫指标检测,CSF的OB、MBP、IgG鞘内合成均正常,不支持多发性硬化诊断。
ADEM伴发视神经炎是儿童病人偶然的临床现象。本组中有4例单眼或双眼视力下降(不伴有脊髓异常信号),其中3例接受视觉诱发电位检测,均明显异常,1例CSF行OB、MBP及IgG抗体检测,未发现异常;随访到3例,均无病情反复、无视物不适感。儿童ADEM继发视神经炎预后良好,转化为多发性硬化的情况少,与KIM等[10]的报道一致。
MOG抗体疾病是新鉴定的中枢神经系统炎症状态[11],发病部位包括视神经、脊髓、脑干和脑。ADEM亦属MOG抗体疾病,因此有必要对ADEM患儿进行CSF和血清的MOG抗体检测。BAUMANN等[12]报道一组33例ADEM患儿,有19例MOG抗体阳性,抗体阳性的患儿除CSF细胞数偏高外,发病年龄、性别及临床症状与阴性患儿均无区别,并发现MOG抗体的存在代表预后良好。本组5例检测CSF及血清MOG抗体,并均成功随访,
CSF均阴性,2例血清阳性,发现血清阳性组与血清阴性组各有1例多相型ADEM患儿,余3例单相病程,无严重后遗症患儿。
儿童ADEM的预后判断困难,研究预后影响因素的文献较少,CSF中OB阳性者复发倾向高[9],MOG抗体阳性患儿预后好[12]。本组资料因检测免疫指标的病例数少,未进行免疫指标对预后影响的统计分析。我们把随访到的41例患儿分为痊愈组和不完全痊愈组,对性别,发病年龄,病前诱因,主要临床症状的肢体活动障碍、惊厥、意识障碍、头痛头晕、发热,CSF白细胞及蛋白水平,四肢肌电图,头颅MRI基底核或脑干病灶的差异进行了统计学分析,探寻这些常见指标是否能预测儿童ADEM的预后,结果显示这些指标2组间差异无统计学意义(P>0.05),不能预测预后。
本组资料属于回顾性研究,基于较多病例数及较长时间随访,可以总结出:儿童ADEM,急性或亚急性起病,脑病样表现,头颅或脊髓MRI异常为其主要诊断依据,大多数经免疫治疗效果良好,少数患儿病情反复或遗留后遗症状,偶有死亡。性别、发病年龄、病前诱因、主要临床症状、CSF白细胞及蛋白水平、四肢肌电图及头颅MRI差异不能预测儿童ADEM的预后。





 DownLoad:
DownLoad: